Practical Tips for Providing Palliative Care in the ED
With Dr. Alisha Benner
ACEP’s 2013 Choosing Wisely campaign identified engaging palliative care or hospice services in the ED as one of their 10 recommendations. Palliative care can help with symptom management, support families and patients, and help clarify their goals of care. Most EDs, however, do not have real-time palliative care consults available at all times, or at all! So the emergency physician is usually the person providing palliative care for patients in the ED. In this episode Alisha Benner discusses what palliative care is and shares pearls for better symptom management, communication with patients, and active management at the end of life.
Defining the Terms
Palliative care, hospice, and DNR are terms that are often misunderstood or conflated. We will start with definitions:
Palliative Care can be provided to anyone who has a serious illness, from the time of diagnosis to end of life. It can be for any age, and during can be provided while curative efforts are underway and when patients are pursuing comfort care. It has 3 main goals:
- To provide active symptom management, along any stage of a serious illness, from onset to end of life, including through both treatments with curative intent and when goals of care have shifted to comfort measures or non-curative treatments.
- To help support the patient and family through the course illness.
- To ensure that the plan of care is in line with the patient’s goals of care and that there is a better understanding between patient and physicians of what those goals are.
Hospice is a specific insurance benefit that provides multi-disciplinary care and 24 hour nurse access for patients who are deemed by 2 physicians to have less than 6 months to live if their illness takes its expected trajectory. Hospice patients are ideally managed at home or the place of their residence (assisted living, skilled nursing, etc), but may need to come to the hospital if their symptoms cannot be managed at their place of residence. It is helpful to call the on-call hospice nurse to coordinate the patient’s care as they may be able to increase the home resources to manage the patient at home. Hospice can be revoked by the patient at any time if they wish to pursue more aggressive treatment.
DNR is a specific order generated by the patient that if their heart went into a non-perfusing rhythm, ie they lost pulses, that they would not want CPR done. It does not necessarily include DNI, although often patients request both DNR and DNI. It also does not imply that they do not want maximal treatment with curative efforts, including IV fluid resuscitation, pressors, central lines, surgery, and ICU admission.
Active Symptom Management
Symptom management is a major part of palliative care. Commonly treated symptoms include pain, nausea, constipation, insomnia, anxiety, dyspnea. Here are pearls for several of these:
Pain
For patients who have chronic pain, such as from cancer or other chronic, painful conditions, first, look for any possible new causes of their pain before attributing it to the underlying chronic pain. You can give IV opioids in the ED to help control their pain, and if needed, can try switching to a different medication. For a patient on 10mg oxycodone Q6hours (40mg total), this would be equivalent to 15mg PO morphine Q6hours (60mg total) assuming complete cross-tolerance. However, there is not complete cross-tolerance, meaning the patient may be less tolerant to morphine, so the dose should be reduced by 25-50%, which would be 7.5mg – 11.2mg Q6hours of morphine PO. The equivalent IV doses can also be calculated for patients who are being treated as inpatients or who are NPO.
Constipation
Treat aggressively and pre-emptively. Avoid Colace because it has very limited, if any, effect, and just increases the stool burden. For patients who are prescribed opioids, with slow down the gut, prescribe Senna, which increases gut motility, 1 tab BID (and can be titrated up), and miralax 1-2 capfuls daily. Both can be used safely long-term. For severe constipation, magnesium citrate can be used in patients without renal failure, as well as enemas or manual disimpaction.
Dyspnea
While treating the underlying cause (eg COPD or CHF exacerbation), very low dose opioids, such as 2.5mg oxycodone PO, or 1mg morphine IV can help reduce the subjective feelings of air hunger and dyspnea, without causing sedation or respiratory depression at these miniscule doses.
Nausea
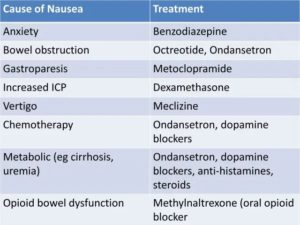
- Zofran is a good go-to for most causes of nausea and vomiting, although like other medications (compazine, reglan) it can prolong the QTc. For specific causes of nausea/vomiting, other agents may be more effective (see table below). For vertigo, phenergan, or meclizine may help better. For migraines, reglan tends to work well. For bowel obstruction, pro-motility agents such as reglan should be avoided, and Zofran or octreotide is likely better. For gastroparesis, by contrast, pro-motility agents may help more. All of them but Zofran will be sedating. Below are the commonly used anti-emetics, with trade name, generic name, and mechanism of action.
- Zofran = ondansetron; 5-HT3 receptor (serotonin) antagonist
- Reglan = metoclopramide; dopamine antagonist, and stimulates upper GI motility, sensitizes to ecetylcholine
- Compazine = prochlorperazine; a 1st gen antipsychotic, dopamine antagonist
- Phenergan = promethazine; central and peripheral histamine antagonist, and anti-cholinergic
- Antivert = meclizine; anti-histamine and anti-cholinergic
- Ativan = lorazepam; binds to and agonizes GABA receptors
- Haldol = haloperidol; 1st gen antipsychotic, dopamine antagonist.
Based on cause of the nausea, different agents may work better. Here are some options, adapted from reference 5.
Delirium
Be aware of it. It can present in a hyperactive form (hallucinations, agitation), hypoactive (may appear depressed or less active), or can be mixed. Delirium is an independent risk factor for 6 month mortality. Always look for an underlying cause!
Delirium PodcastCommunicating With Families
Gaining an overall picture of how the patient has been doing in the last months to year can be incredibly helpful in discussing options with the family and goals of care and does not take much pain. Our goal is to help support the family and patient in their decisions, while making sure they understand the options and the risks and benefits. Reference 3 has some great advice.
Active Management at the End of Life
At the end of life, it is important to let patients and families know that just because curative efforts have ended or are unlikely to be effective that we as medical caregivers are not abandoning them, but will continue to actively manage their symptoms. Start by assessing their symptoms. See reference 4 for a more in-depth discussion, but here are a few medications that can help for common symptoms:
Opioids: Are helpful for pain, dyspnea, and cough, starting at a low dose, and titrating up as needed and depending on the goals of care and patient wishes. Some patients may want to be less sedated to communicate with family and will tolerate more pain or dyspnea. Others may want to reduce their pain even if it causes sedation.
Benzodiazepines: Can help with anxiety, myoclonic twitching, hiccups, insomnia.
Haloperidol: Can help with agitation, nausea, hallucinations:
Scopolamine patches: Can help with respiratory secretions. Other options include 1% atropine eye drops under the tongue Q8 hours, or glycopyrrolate 1mg PO or 0.2mg IV.
Relieving the Existential Suffering
Being diagnosed with or suffering from a severe illness can cause emotional stress, loss of sense of self, anxiety, depression, and fear. One way to help connect with patients is to make sure you sit down and take time to listen to them and their concerns. “Wish, Worry, Hope” statements such as “I wish things were different” or “I worry that the current treatment is not working”. Acknowledging that they have been suffering with a disease process if that is something they communicate to you, can also help validate them. Leave space for silence as patients process new information or diagnoses, or process their own thoughts.
References
- Ebell MH, Jang W, Shen Y, Geocadin RG, Get With the Guidelines-Resuscitation Investigators. Development and validation of the good outcome following attempted resuscitation (GO-FAR) score to predict neurologically intact survival after in-hospital cardiopulmonary resuscitation. JAMA Intern Med. 2013;173(20):1872-1878. https://www.ncbi.nlm.nih.gov/pubmed/24018585
- Ohlsson MA, Kennedy LM, Ebell MH, Juhlin T, Melander O. Validation of the good outcome following attempted resuscitation score on in-hospital cardiac arrest in southern sweden. Int J Cardiol. 2016;221:294-297. https://www.ncbi.nlm.nih.gov/pubmed/ 27404694
- Ngo-Metzger Q, August KJ, Srinivasan M, Liao S, Meyskens FL,Jr. End-of-life care: Guidelines for patient-centered communication. Am Fam Physician. 2008;77(2):167-174. https://www.ncbi.nlm.nih.gov/pubmed/ 18246886
- Groninger H, Vijayan J. Pharmacologic management of pain at the end of life. Am Fam Physician. 2014;90(1):26-32. https://www.ncbi.nlm.nih.gov/pubmed/ 25077499
- Clary PL, Lawson P. Pharmacologic pearls for end-of-life care. Am Fam Physician. 2009;79(12):1059-1065. https://www.ncbi.nlm.nih.gov/pubmed/ 19530636
- Opioid Dosage Conversion phone app
- Palliative Care Fast Facts phone app
- Many resources and articles are available here from the American Association of Family Physicians
- Good Outcome Following Attempted Resuscitation (GO-FAR) Calculator
This podcast uses sounds from freesound.org by Jobro and HerbertBoland
Image credit [1]
This entry was posted in Palliative Care. Bookmark the permalink.
Hosted by
Dr. Christina Shenvi is an associate professor of Emergency Medicine at the University of North Carolina. She is fellowship-trained in Geriatric Emergency Medicine and is the founder of GEMCast. She is the director of the UNC Office of Academic Excellence, president of the Association of Professional Women in Medical Sciences, co-directs the ACEP/CORD Teaching Fellowship, is on the Annals of EM editorial board, is on the Geriatric ED Accreditation board of governors, and she teaches and writes about time management at timeforyourlife.org.