Geriatric ED Quality Improvement SBAR: Post ED Orders in a Large Health Care System at Multiple EDs
Situation
The rate of post-ED (emergency department) orders for PCP (primary care providers), Homecare, Physical Therapy consults in the ED, and Out patient Physical Therapy is low for discharged community-dwelling older adults visiting the ED, resulting in a higher rate of revisits.
The goal is to increase the rate of post-ED orders for discharged at-risk community-dwelling older adults.
Background
The Geri ED program was developed to identify at-risk community-dwelling older adults visiting the ED, change their trajectory (reduce revisits & admissions) and return them back to the community by connecting the patient with resources outside the ED.
Geri ED Dashboard
With the advent of the Geri ED Dashboard, we can identify a correlation between low post-ED service orders rates and higher revisit rates for older community-dwelling fallen patients. A structured comparison between sites was developed to highlight this correlation. Currently, the Geri ED program has been implemented and accredited (ACEP Level III accreditation) at 15 of 24 sites. The remaining 9 sites will be implemented and accredited by 2023. One of these 15 sites has ascended to ACEP Level II Geri ED accreditation, which is the first in Wisconsin & Illinois. As part of this site’s goal of improving care for vulnerable older adults, they have significantly increased post-ED service orders.
15 Geri ED site high risk QI study
Usual Care Inclusion criteria
- 14 ED sites that have implemented Geri ED
Usual Care Exclusion criteria:
- 3 sites = < 50% ISAR completion 9 sites = not implemented Geri ED at time of SBAR Comparison Inclusion criteria 1 site = high rate of service to orders (>45% post ED service orders)
High Risk Population characteristics (all sites):
- 2020 data, >3 ISAR, <3 ESI, >65 years old, discharged, Chief Complaint and/or Clinical Impression of Fall
Assessment
The results of the two group comparison strongly suggests an inverse correlation between a low rate of recidivism and high rate of post ED service orders for high risk community dwelling older adults visiting the ED with a fall.
Usual Care group (twelve Level III Geri EDs):
- n= 880 visits
- 6.5% visits with a post ED service order
- 31.6% 30 day revisits,
- 8.5% 72hrs revisit
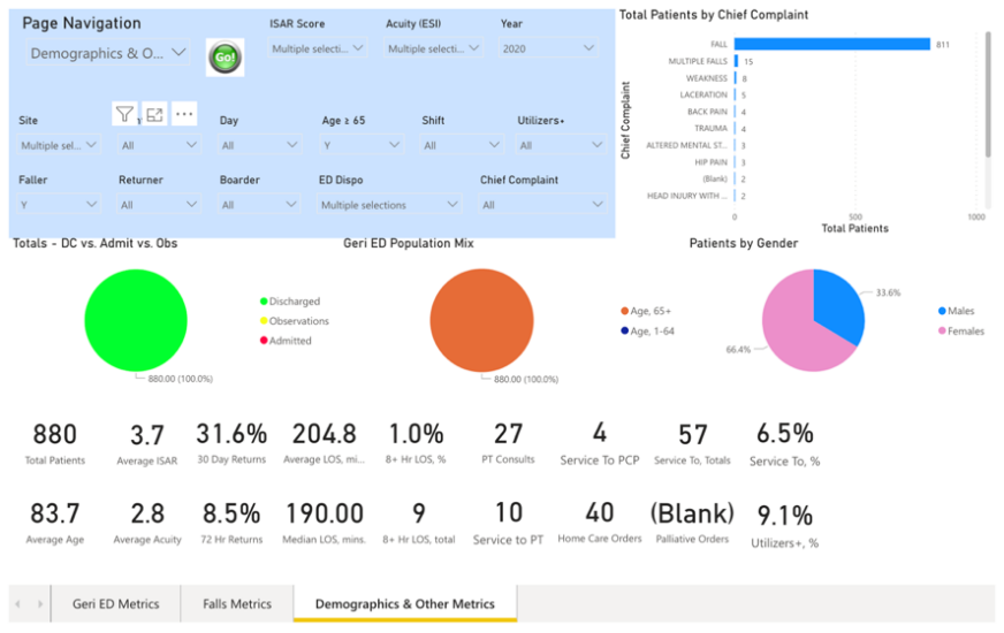 Geri ED Dashboard Screen shot: 12 ED site Group (Usual Care group)
Geri ED Dashboard Screen shot: 12 ED site Group (Usual Care group)
Comparison group (one Level II Geri ED):
- n= 127 visits
- 47.2% visits with a post ED service order
- 22.0% 30 day revisits,
- 3.9% 72hr revisits
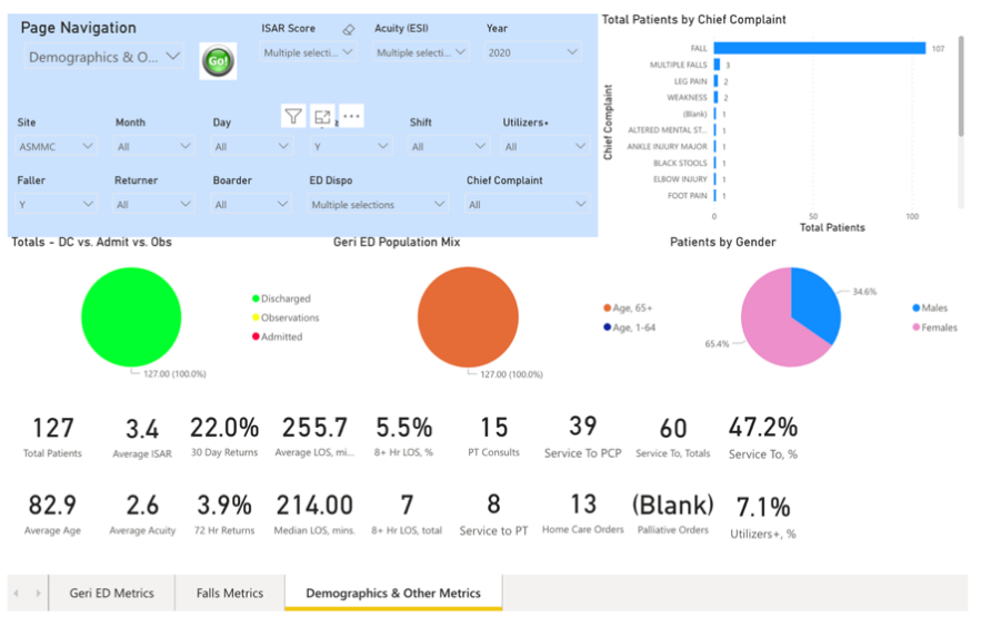 Geri ED Dashboard Screen shot: 12 ED site Group (Usual Care group)
Geri ED Dashboard Screen shot: 12 ED site Group (Usual Care group)
Recommendation
The Geri ED program makes the following recommendations to decrease rate of ED revisits by increasing rate of post ED service orders:
Collaborate with System Emergency Medicine, Nursing, Care Management, Rehab, and Population Health
- Present findings to system Joint ED Leadership committee
- Analyze patterns of practice
- Identify barriers and opportunities for order placement
- Develop standardized criteria for placing post ED service orders
- Implement system wide ED education
- Develop metric tracking and communication plan
- Reach concensus on placing orders.
- PCP ordering
- Resolve issue of one order for two different intentions
- Establish new PCP provider relationship verses setting follow-up appointment post ED.
- Develop mechanism for actively setting follow-up PCP appointments prior to ED disposition verses the current passive PCP follow-up ‘instructions’ in AVS (after visit summary)
- Resolve issue of one order for two different intentions
- PCP ordering
Create & implement an automated decision support function for providers in ED in the EHR
- Identify parameters for trigger
- Receive feedback and eventual approval from stakeholder committees
- Build and implement trigger
- Direct link to the suggested order
Setting: Large integrated health care system in the northern mid-west of the United States
Definitions:
- ISAR= Identification of Seniors at Risk tool
- ESI= Emergency Severity Index
- Post-ED orders:
- PCP= Primary Care Providers, Internal Medicine, Family Practice
- Homecare= Homecare
- PT Orders= Physical Therapy consults in the Emergency Department
- Service to PT= Out patient Physical Therapy
Contributing Faculty
Aaron Malsch is the Senior Services Program Manager at AdvocateAuroraHealth (AAH) in Wisconsin & Illinois. He supports several geriatric models of care (NICHE, Geri ED, HELP, ACE Tracker, Geriatric Scholars). His focus is on nursing and interprofessional practice as it relates to the elder population throughout the AAH system of clinics, hospitals, emergency departments, home care services, and long term setting partners. In support of these models of care, Aaron has developed expertise in developing EHR workflow tools and reports to facilitate front line staff’s efforts and demonstrate outcomes. He leads the Geriatric ED implementation and achieved ACEP Geri ED accreditation at all AAH EDs. Aaron contributes nationally to the improvement of care for older adults, highlighted by being Chair of the geriatric committee at the Emergency Nurses Association (ENA), co-planner of GEDC symposium at the ENA conference, and reviewer of Geriatric ED Accreditation program at ACEP.