Using the 4M Model to Screen Geriatric Patients in the Emergency Department
Volume 2 | Issue 3 | Article 2 - Review Article
Full TextIntroduction
Older adults represent about 1 in 5 patients in the Emergency Department (ED) setting.1 The ED may be the first or only point of health care contact for some older patients. Treating this population often requires the ED physician to take a multidisciplinary approach and to ensure a plan for continuity of care, in addition to the usual ED emergent evaluation. Often, these patients are also experiencing complex social or functional challenges at home, which may make accessing healthcare options difficult for them. This presents an important screening opportunity for providers with a goal of preventing future illness or injury in older patients.
Southerland et al. describe various models of geriatric care in the ED.2 These models are all rooted in focused, multidisciplinary care aimed specifically at the geriatric population. Several screening tools have been developed to assess which older ED patients are at higher risk. However, the screening tools are highly variable and depend on many factors including ED capacity and staffing. In addition, existing screening tools may not be adequate to accurately distinguish high-risk from low-risk older patients.3
In recognition of the complexity of care of the older patient and prevention opportunities, the American College of Emergency Physicians (ACEP) has created a geriatric care quality accreditation program with designated levels of geriatric ED quality. In 2019, our ED became the 10th ED to receive ACEP’s Geriatric ED (GEDA) level-1 accreditation. We are a suburban, academic ED with an annual volume of approximately 123,000 patients with 28% of patients age 65 or older. During the GEDA accreditation process, we aimed to create a tool that could simplify and standardize the care of our older patients. This screening tool was designed for use by attending physicians, resident physicians, advanced nurse practitioners, physician assistants, ED nursing staff, and students. We also planned to implement our nursing team’s screening efforts to be incorporated into our ED provider’s note in the electronic health record (EHR). Finally, we aimed to have ED providers document when a patient met criteria for continued specialized Geriatric consultative services, either as an inpatient or as an outpatient. In order to provide simple, standard communication we created a screening model based on the 4M model of geriatric care that would trigger an indication for referral to a geriatrician. The purpose of this paper is to outline a screening method we have developed based on the geriatric 4M model for older patients presenting to the ED. This screening tool is used to identify patients who may benefit from referral to specialized geriatrics care. Once implemented, we hope to use this screen in the future to track data of referred patients longitudinally in order to both identify high risk features of these patients, fine tune the screening method, and track outcomes of those patients referred.
The 4M Model
Our geriatric ED goal is to first identify patients who would benefit from referral to specialized care by a geriatrician, and then assist in streamlining that process. We use the 4M Model for Creating Age-Friendly Health Systems as a model for a geriatric screening tool that is included in our EHR. The 4M Model was developed by the Institute for Healthcare Improvement (IHI) to provide high-quality care to older adults through the following four elements: Mentation, Mobility, Medications, and What Matters.4
Each of the four components of the 4M model are addressed as assessment items within the screening tool that is pre-populated in the EHR by using a “smart phrase” (.GERI4M). The smart phrase is a function that allows the user to instantly bring up the 4M screen and all of its components in the EHR. Providers can then perform the screen at bedside and document that it was included as part of the ED visit. In addition, a geriatric referral may be triggered if necessary. These components, as well as the associated assessment tools, are displayed in Figure 1.
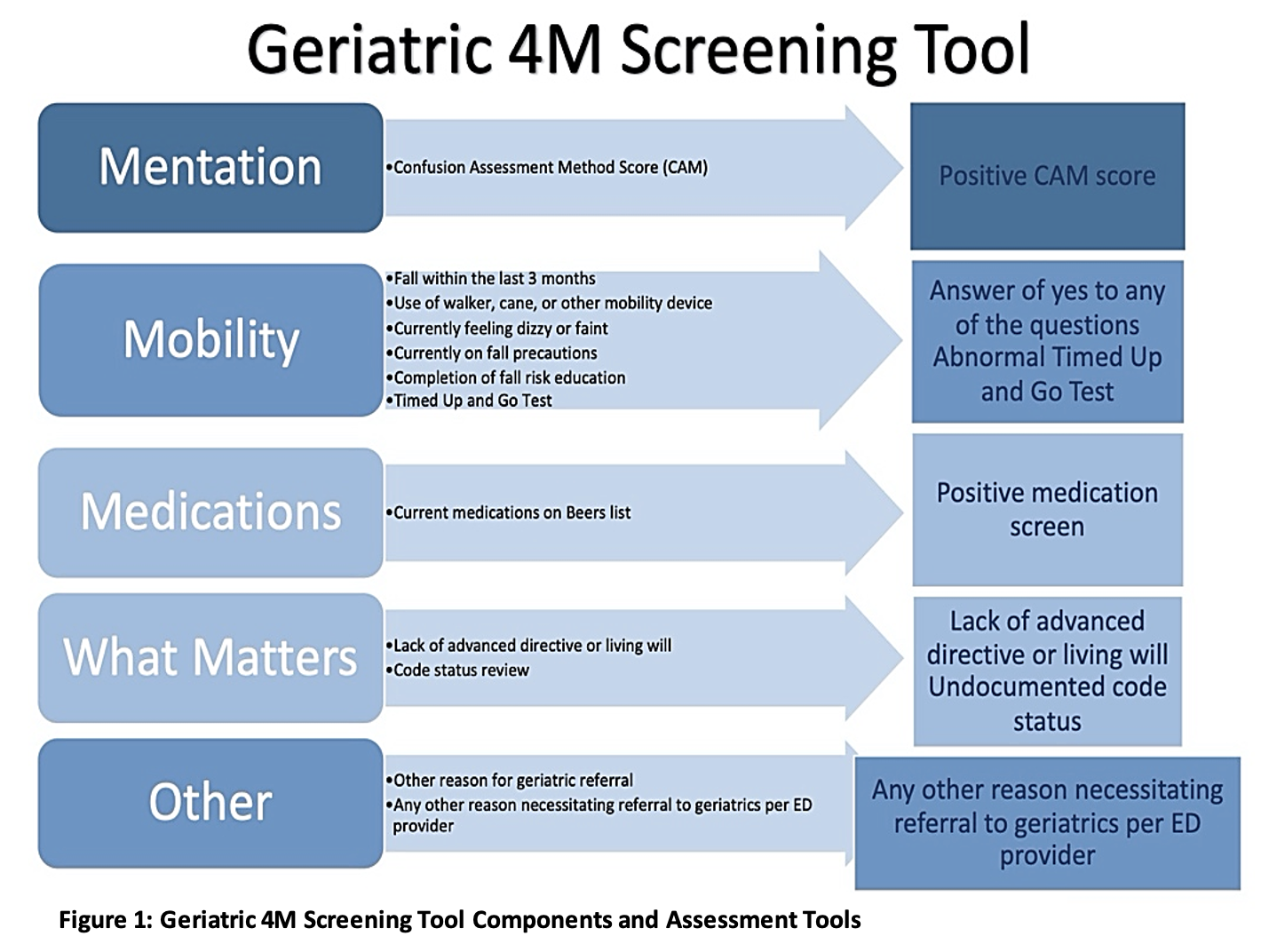
- Mentation is evaluated using the Confusion Assessment Method (CAM) Score to screen for delirium. The CAM score has been cited as a potential reference standard for emergency department use.5 A systematic review of 22 delirium screening studies found that delirium was most often reported at a rate of 7-10% for older adults presenting to the ED and often goes unnoticed.6 The presence of delirium upon presentation to the emergency department has been shown to be associated with a significantly higher 6-month mortality.7 Identification of delirium as part of the 4M screen is an important screen as it is often missed in the ED setting.
- Mobility assessment includes a series of questions regarding history of falls within the past 3months, use of mobility aids, presence of dizziness or faintness at presentation, use of fall precautions, and completion of patient fall risk education. The timed up and go (TUG) test is included, as it has been shown to be a relatively sensitive and specific tool to detect fall risk in older adult.8,9 Including fall screening and a TUG test as part of the mobility assessment in the screen allows for identification of those patients at higher risk for falls at time of presentation and coordination of care with a geriatrician and a physical therapist, as an inpatient or outpatient.
- Medication screening involves provider review to see if any medications are on the Beers list as noted by the American Geriatrics Society.10 This list seeks to identify medication use that is potentially inappropriate for older adults. ED providers have point of care access to the Beers criteria to quickly identify medications on this list.
- Finally, an assessment of What Matters to the older patient provides individualized care. We selected to screen for the presence of an advanced directive or living will and verification of the patient’s code status. Patients who lack an advanced directive or living will receive a positive screen. This allows us to facilitate end of life goal discussions either in the ED setting or as follow up with the Geriatrician.
The 4M Screening Tool
Geriatric screening using the 4M model helps identification of patients at risk for further illness or injury. Second, it initiates a process for transitions of care to the Geriatric team. We use this same screening tool for those older patients who are admitted to the hospital and those who are discharged from the ED. Additionally, if physical therapy, occupational therapy, or social work referral is needed, that can be ordered in the ED setting either to be initiated acutely or as outpatient follow up.
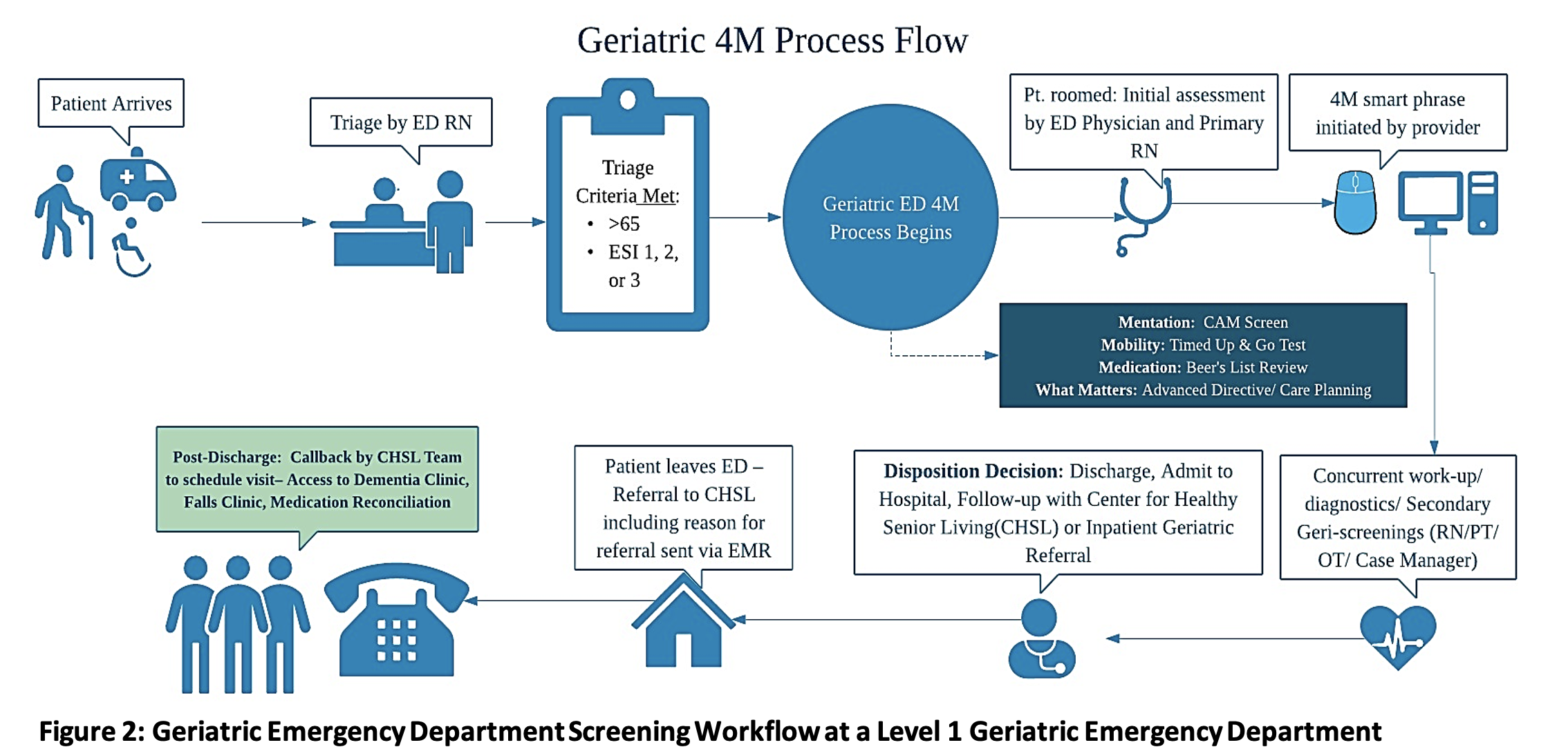 Legend: ED = Emergency Department. RN = Registered Nurse. ESI = Emergency Severity Index. Pt = Patient. PT = Physical Therapy. OT = Occupational Therapy
Legend: ED = Emergency Department. RN = Registered Nurse. ESI = Emergency Severity Index. Pt = Patient. PT = Physical Therapy. OT = Occupational Therapy
The ED process for screening older patients is displayed in Figure 2. Information is initially obtained by nursing staff and then transferred directly into the screening tool questions. ED providers then document a “.GERI4M” section in their note and fill in any missing information in the smart phrase. Any positive 4M screen is an indication for referral to Geriatrics. These referrals are either inpatient or outpatient depending on the patient’s disposition after their ED visit. Our geriatrics team, which includes a board-certified Geriatrician and her staff, receives an instant message about the referral which is automatically triggered by a positive 4M screen. The geriatric team will then call the patient directly to make an appointment for outpatient follow up. If the patient is being admitted, the positive 4M screen automatically triggers an order for inpatient consultation by Geriatrics, which expedites and ensures the inpatient visit.
Automating the referral process is critical as older patients presenting to the ED are often lost to follow up or re-hospitalized for a variety of reasons including not fully understanding their discharge instructions.11,12 Various efforts to improve elderly patient adherence with follow up after visits to the ED have proven unsuccessful.13,14 These patients may also be at increased risk of death or ICU admission depending on several factors including change in disposition and cognitive impairment6, further necessitating the need to ensure adequate follow up.
Limitations
There are some limitations to using the 4M model as a screening tool. One is that the Beers list of medication is quite extensive, and we currently do not have an automated tool in the EHR to screen for these medications. Implementation of this medication list directly into the EHR may help facilitate its integration as a screening tool. In addition, there may be alternate components related to medication such as polypharmacy that could be used as an adjunct to our current criteria.
Another limitation is in the nursing workflow required to evaluate these patients. Although the majority of the information is easily obtained, there are certain parts that prove to be more cumbersome. For instance, some of the nursing staff do not feel comfortable routinely using some of the assessment tools such as the CAM delirium screen or TUG test, especially when the patient may be fatigued or severely ill. The lack of screening may be problematic as delirium has been shown to be unrecognized in greater than 50% of cases.15 Although CAM has been suggested to be a possible reference standard in screening for delirium in the ED, research on its frequency of utilization is limited.
Some of these screening components require more time and effort than others, which is a barrier for nurses in a busy ED. Efforts have been made to simplify the tool and allow it to be integrated seamlessly into the intake process for all older patients in the ED. For example, using a modified version of CAM, such as the “Brief Confusion Assessment Method,” may help to ensure that this screening is performed on most patients.16–18 One final limitation is that certain patients may be incapacitated, and complete screening may not be feasible.
Conclusion: Future Considerations and Implementation Across Other Eds
Further studies are needed to assess and quantify the impact of geriatric screening tools. In particular, future research regarding the 4M screening tool will include an analysis of the total number of patients screened, number of patients who screen positive, and outcomes for those receiving a geriatric specialty referral. Ultimately, the goal should be to measure if these geriatric referrals result in reduced readmissions and improved morbidity and mortality. Obtaining such outcome data may demonstrate a return of investment for additional geriatric resources.19–21
A screening tool based on the 4M model is feasible to implement at a level 1 Geriatric ED. The tool is designed to help identify older patients who require additional specialty care. In addition, it may help provide a standard referral process. The geriatric population is a vulnerable population who cannot necessarily advocate for themselves, particularly in the ED setting. Having a standardized ED screening tool like the 4M screen will hopefully improve care overall for older patients.
Key Words
Geriatric, Screening, 4M model, Referral, Geriatric Emergency Department
Acknowledgements
Corresponding Authors:
- Douglas Finefrock, DO; dougfinefrock11@gmail.com
- Martinus Megalla, BA martinus.megalla@gmail.com
Author Contributions: All authors listed have participated in the drafting and editing of this manuscript.
Conflicts of Interest: All authors have no conflicts of interest to disclose.
Sponsor’s Roles: None to report
Affiliations
Martinus Megalla, BA
- Department of Emergency Medicine, Hackensack Meridian School of Medicine, Nutley, NJ, USA
- Department of Emergency Medicine, Hackensack University Medical Center, Hackensack, NJ, USA
Roopa Avula, MD
- Department of Emergency Medicine, Hackensack University Medical Center, Hackensack, NJ, USA
Christopher Manners BA
- Department of Emergency Medicine, Hackensack Meridian School of Medicine, Nutley, NJ, USA
- Department of Emergency Medicine, Hackensack University Medical Center, Hackensack, NJ, USA
Portia Chinnery, RN
- Department of Patient Safety and Quality, Hackensack Meridian Health, Hackensack, NJ, USA
Lindsey Perrella, RN
- Department of Patient Safety and Quality, Hackensack Meridian Health, Hackensack, NJ, USA
Douglas Finefrock, DO
- Department of Emergency Medicine, Hackensack Meridian School of Medicine, Nutley, NJ, USA
- Department of Emergency Medicine, Hackensack University Medical Center, Hackensack, NJ, USA
References
- Ashman JJ, Schappert SM, Santo L. Emergency Department Visits Among Adults Aged 60 and Over: United States, 2014-2017. NCHS Data Brief. 2020;(367):1-8.
- Southerland LT, Lo AX, Biese K, et al. Concepts in Practice: Geriatric Emergency Departments. Annals of Emergency Medicine. 2020;75(2):162-170. doi:10.1016/j.annemergmed.2019.08.430
- Carpenter CR, Shelton E, Fowler S, et al. Risk Factors and Screening Instruments to Predict Adverse Outcomes for Undifferentiated Older Emergency Department Patients: A Systematic Review and Meta-analysis. Academic Emergency Medicine. 2015;22(1):1-21. doi:https://doi.org/10.1111/acem.12569
- What Is an Age-Friendly Health System? | IHI – Institute for Healthcare Improvement. Accessed December 30, 2020. http://www.ihi.org:80/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx
- Mariz J, Costa Castanho T, Teixeira J, Sousa N, Correia Santos N. Delirium Diagnostic and Screening Instruments in the Emergency Department: An Up-to-Date Systematic Review. Geriatrics (Basel). 2016;1(3). doi:10.3390/geriatrics1030022
- LaMantia MA, Messina FC, Hobgood CD, Miller DK. Screening for Delirium in the Emergency Department: A Systematic Review. Annals of Emergency Medicine. 2014;63(5):551-560.e2. doi:10.1016/j.annemergmed.2013.11.010
- Han JH, Shintani A, Eden S, et al. Delirium in the Emergency Department: An Independent Predictor of Death Within 6 Months. Annals of Emergency Medicine. 2010;56(3):244-252.e1. doi:10.1016/j.annemergmed.2010.03.003
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148. doi:10.1111/j.1532-5415.1991.tb01616.x
- Shumway-Cook A, Brauer S, Woollacott M. Predicting the Probability for Falls in Community-Dwelling Older Adults Using the Timed Up & Go Test. Physical Therapy. 2000;80(9):896-903. doi:10.1093/ptj/80.9.896
- Croke LM. Beers Criteria for Inappropriate Medication Use in Older Patients: An Update from the AGS. AFP. 2020;101(1):56-57.
- Engel KG, Buckley BA, Forth VE, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest? Acad Emerg Med. 2012;19(9):E1035-1044. doi:10.1111/j.1553-2712.2012.01425.x
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. doi:10.1056/NEJMsa0803563
- Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone Follow-Up for Older Adults Discharged to Home from the Emergency Department: A Pragmatic Randomized Controlled Trial. J Am Geriatr Soc. 2018;66(3):452-458. doi:10.1111/jgs.15142
- Nasser L, Stratton T. BET 1: Follow-up phone calls and compliance with discharge instructions in elderly patients discharged from the emergency department. Emergency Medicine Journal : EMJ. 2019;36(2):126. doi:http://dx.doi.org/10.1136/emermed-2019-208441.1
- Boucher V, Lamontagne M-E, Nadeau A, et al. Unrecognized Incident Delirium in Older Emergency Department Patients. J Emerg Med. 2019;57(4):535-542. doi:10.1016/j.jemermed.2019.05.024
- Wilson JE, Boehm L, Samuels LR, et al. Use of the brief Confusion Assessment Method in a veteran palliative care population: A pilot validation study. Palliat Support Care. 2019;17(5):569-573. doi:10.1017/S1478951518001050
- Baten V, Busch H-J, Busche C, et al. Validation of the Brief Confusion Assessment Method for Screening Delirium in Elderly Medical Patients in a German Emergency Department. Acad Emerg Med. 2018;25(11):1251-1262. doi:10.1111/acem.13449
- Han JH, Wilson A, Graves AJ, Shintani A, Schnelle JF, Ely EW. A Quick and Easy Delirium Assessment for Non-Physician Research Personnel. Am J Emerg Med. 2016;34(6):1031-1036. doi:10.1016/j.ajem.2016.02.069
- Southerland LT, Savage EL, Muska Duff K, et al. Hospital Costs and Reimbursement Model for a Geriatric Emergency Department. Acad Emerg Med. 2020;27(10):1051-1058. doi:10.1111/acem.13998
- Pines JM, Edginton S, Aldeen AZ. What We Can Do To Justify Hospital Investment in Geriatric Emergency Departments. Academic Emergency Medicine. 2020;27(10):1074-1076. doi:https://doi.org/10.1111/acem.13999
- Hwang U, Dresden SM, Rosenberg MS, et al. Geriatric Emergency Department Innovations: Transitional Care Nurses and Hospital Use. J Am Geriatr Soc. 2018;66(3):459-466. doi:10.1111/jgs.15235