This webinar has completed and is available on-demand. Please see below for supporting materials and webinar recording.
Overview
Experts discuss strategies for eliciting patient healthcare goals in an emergency setting with complex older patients, and how emergency departments can meet domain one of the CMS Age-Friendly Hospital Measure.
Goals
- Introduce CMS Age-Friendly Measure Domain 1 and its impact on ED care for older adults.
- Share practical strategies and real-world examples for eliciting patient healthcare goals in emergency settings in the U.S. and beyond.
- Hear from experts in the field about how they integrate goals of care in their ED workflow.
Webinar Resources
Slide Deck
October 27, 2025
This powerpoint deck includes summary slides and the key points from each presenter.
On-Demand Webinar Recording
October 27, 2025
The webinar recording can be found on YouTube.
Transcript
October 27, 2025
Click below to download the transcript from the recording.
Related Resources
Below are some resources mentioned in the webinar by our panelists which you may find helpful.
CMS Age Friendly Hospital Measure: Resources for Emergency Departments
August 28, 2024
Helpful educational resources put together by the GEDC team to help you and your emergency department meet the CMS Age-Friendly Hospital measure.
Condensed Conversation Guide for Identifying Patient Priorities (The One Thing) Emergency Department Version
Printable PDF from Patient Priorities
A free, printable conversation guide for use by ED clinicians developed by Patient Priorities Care Initiative in collaboration with Age-Friendly Health System initiative of the Institute for Healthcare Improvement.
A Qualitative Study of “What Matters” to Older Adults in the Emergency Department
July 1, 2022
A qualitative study by panelist Cameron Gettel, MD, MHS, using semi-structured interviews to seek out themes amongst concerns and desired outcomes of older patients in the ED.
A Qualitative Study of Health Priorities of People With Dementia and Care Partners in Emergency Department and Hospital Care in a Public Safety-Net Setting
October 4, 2025
An interview-based study by panelist Anita Chary, MD, PhD on the perspectives and priorities of older adults presenting to the ED with dementia.
Included in this study are some suggested modifications of the ED patient priorities care (PPC) framework for people with dementia and their caregivers. They are shown below.
| Original scripts and questions | Questions for people with dementia | Questions for care partners |
|---|---|---|
| Patient priorities care for the emergency department | ||
| Introduction | ||
| “In our ED, we want to understand what matters to you about health and your healthcare, to make sure that the care we give during your time in the ED, as well as after discharge, is right for you.” | “I want to ask you a few questions. I want to make sure we address your biggest concern today.” | “I want to ask a few questions to make sure we address your biggest concern today.”“We want to ask you a few questions to make sure [name of patient’s] care focuses on what matters most to them and to you.” |
| Establishing patient or care partner’s priority in the acute care setting | ||
| “What concerns you most when you think about your health and about being in the ED today/tonight?”“What fears and worries do you have about your health as you think about what brought you to the ED today/tonight?” | “What is your biggest worry today?” | “What is your biggest worry about [name of patient’s] health today?” |
| Proximal outcome goal in acute setting | ||
| “What outcome are you most hoping for from this ED visit?” | “What are you most hoping for from this ED visit?”“What are your symptoms getting in the way of? How do you hope this ED visit can help with that?” | “What are [patient name’s] symptoms getting in the way of? How do you hope this ED visit can help with that?”“What are you most hoping comes out of this ED visit?”Consider prompting patient and/or care partner regarding hopes about:Establishing a diagnosisObtaining reassuranceControlling an acute symptomCoordinating care |
| Ancillary questions to facilitate decision-making about hospital admission | ||
| In scenarios of clinical equipoise, that is, condition can be reasonably treated in outpatient or inpatient settingCare preferences: Based on what we’ve found today, we could treat you [patient name] here in the hospital or at home with follow-up. Do you have a preference?Caregiving context: While you [patient name] recover[s], you [patient name] might need help with day-to-day activities. Are there people who live with you [patient name] or who could come to [patient name] to help with this?Follow-up care: Do you [patient name] have a doctor you see regularly? How easy or hard would it be to follow up with them in a few days?In scenarios where clinician recommends inpatient admissionI recommend that you [patient name] stay in the hospital for [monitoring, treatment]. My goal for the hospital admission is [name the specific problem/issue that admission will address, tie back to patient/care partner’s biggest health concern and desired outcome when possible].Example: “My goal for the hospital admission is to take off fluid. We want to make sure the leg swelling goes down enough for Mr. X to be able to walk around at home without needing oxygen.” | ||
Note: This table is taken directly from A Qualitative Study of Health Priorities of People With Dementia and Care Partners in Emergency Department and Hospital Care in a Public Safety-Net Setting, Accessed October 28, 2025. https://agsjournals.onlinelibrary.wiley.com/doi/10.1111/jgs.70136.
Designing a Best Possible Caregiver History to Facilitate Disposition Planning for Older Adults in Emergency Departments
September 30, 2024
A Veterans Affairs study that developed a standardized format called a “Best Possible Caregiver History”, a tool ED clinicians can use to guide disposition decisions from the ED.
Eliciting Healthcare Goals in the ED
October 22, 2025
New GEDC blog authored by panelist Dr. Anita Chary outlining some simple considerations for clinicians about asking patients about their healthcare goals.
What matters most in acute care: an interview study with older people living with frailty
February 25, 2022
This figure, from panelist James van Oppen’s study, highlights acute healthcare goals among older patients living with frailty.
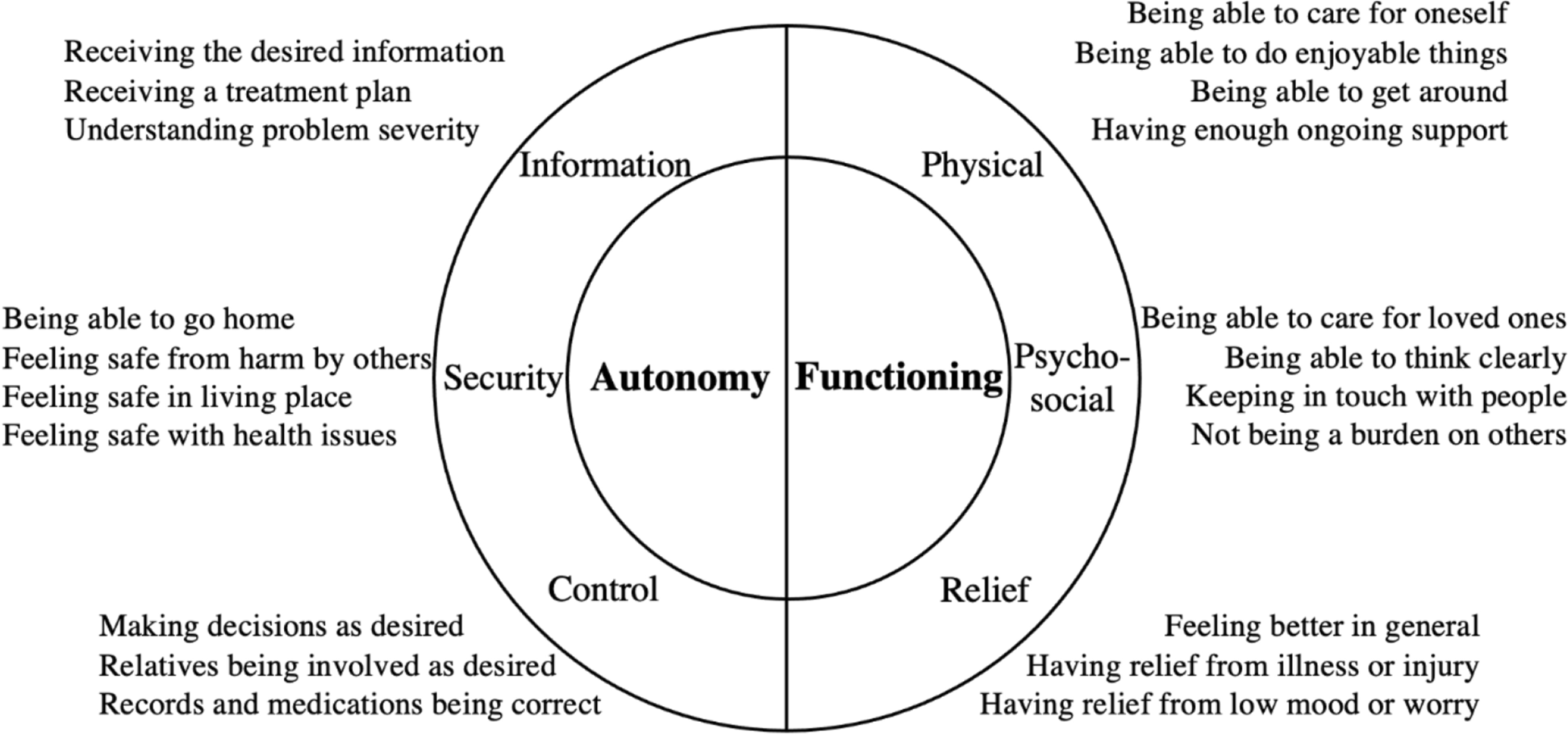
Note: This figure is taken directly from What matters most in acute care: an interview study with older people living with frailty, Accessed October 28, 2025. https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-022-02798-x.
PROM-OPAC Tool
Healthcare outcome measure for older patients living with frailty receiving ED care, developed and validated between 2020-2024. Linked below is the website as well as two studies validating the PROM-OPAC.
Panelists
Susan Bower, MSN, RN
RST Emergency Department Geriatric Nurse Coordinator
Assistant Professor of Nursing
Mayo Clinic
Anita Chary, MD, PhD
Assistant Professor
Associate Director, Medical Scientist Training Program, Baylor College of Medicine
Assistant Research Director, Henry J.N. Taub Department of Emergency Medicine
Section of Health Services Research, Department of Medicine, Baylor College of Medicine
Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center
Cameron Gettel, MD, MHS
Assistant Professor
Clinical Investigator, Center for Outcomes Research and Evaluation (CORE)
Department of Emergency Medicine
Yale University School of Medicine
James van Oppen, FRCEM, MRCP, PhD
NIHR Clinical Lecturer in Emergency Medicine
University of Sheffield & Sheffield Teaching Hospitals NHS Trust
Sheffield, England, United Kingdom
Jessica Stanich, MD
Assistant Professor of Emergency Medicine
Geriatric Medical Director | Department of Emergency Medicine
Joint appointment Department of Medicine, Section of Geriatric Medicine
Mayo Clinic


