The origins of GEDC and GEAR
Early 1990’s
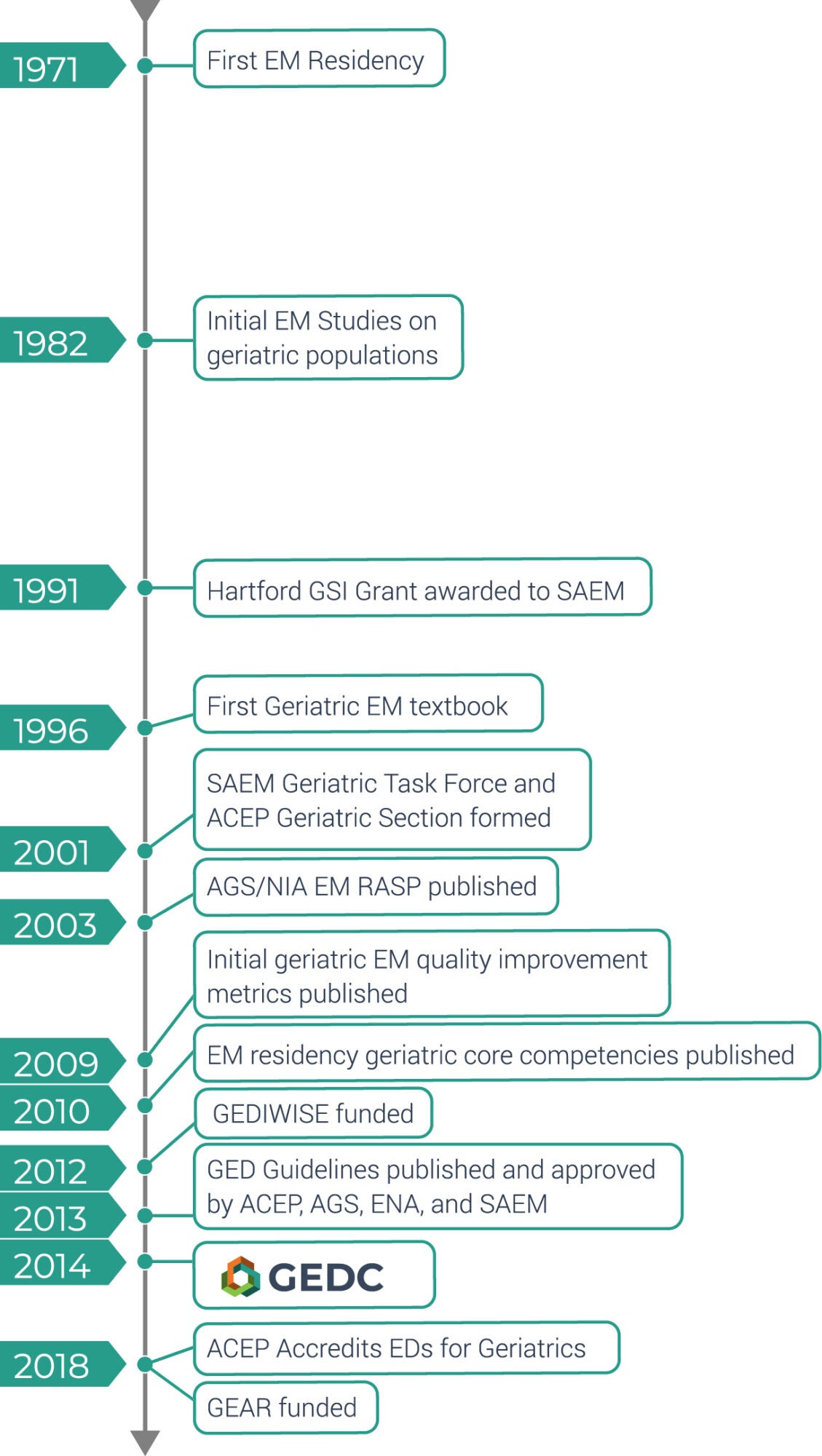
Research beginning in the early 1990s catalyzed the creation of GEDC. During that time, the American Geriatrics Society (AGS) editorialized about a looming shortage of Geriatricians to address aging Baby Boomers. The John A. Hartford Foundation funded the Society for Academic Emergency Medicine (SAEM) to explore issues related to emergency care of older adults. This funding led investigators to a series of studies that focused on the uniqueness of geriatric emergency department utilization and experience of care,1-3 emergency physician perspectives,4 future resident trainee requirements,5 and projected epidemiology of older adult emergency care.6 One overarching observation of these studies was the recognition that more research was required and the momentum catalyzed the birth of a “Geriatric Emergency Medicine Interest Group” (now the Academy of Geriatric Emergency Medicine) within SAEM and shortly thereafter the Geriatric Emergency Medicine Section within the American College of Emergency Physicians.
Early 2000’s
By the early 2000s, the Hartford Foundation had created the Jahnigen Career Development Award across surgical specialties (of which emergency medicine was one). The Jahnigen and Beeson Awards fueled growth of early stage emergency medicine investigators into mature researchers and leaders within organized medicine.7 Along the way, geriatric emergency medicine education and clinical research leaders expanded knowledge across the spectrum of care, including:
- Quality indicators for high-quality geriatric emergency care.8
- High priority research foci.9,10
- Trainee perspectives and core competencies for emergency medicine residents.11,12
- Scoping reviews of the status quo in geriatric emergency care.13,14
- Multiple textbooks15-19 and textbook chapters20-22 devoted to the unique challenges of providing efficient, high quality, evidence-based, and patient-centric emergency care for aging adults.
2007
In 2007, Ula Hwang’s seminal article hypothesized about the concept of a “Geriatric Emergency Department”.23 Subsequently, geriatric emergency medicine opinion leaders and key stakeholders created the Geriatric Emergency Department Guidelines to provide specific recommendations and measurable outcomes for older adult emergency care.24
ACEP, SAEM, AGS, and the Emergency Nurses Association (ENA) quickly endorsed these guidelines and the Canadian Association of Emergency Physicians, American Academy of Emergency Medicine, and American College of Osteopathy Emergency Physicians later endorsed these same guidelines.
The International Federation for Emergency Medicine published an adapted version of the guidelines for more austere settings.25
2007-2018
Early healthcare outcomes research exploring the potential benefits and harms of adherence to components of these guidelines provided mixed results. For examples, research demonstrated reductions in high-risk medication prescribing via an interdisciplinary med reconciliation process including academic detailing,26,27 preventing a portion of emergency department returns using transitional care nurses,28 but no benefit of nurse telephone follow-up as a preventative intervention29,30 or for any vulnerability screening instrument.31
2018
In 2018, the Geriatric Emergency care Applied Research Network (GEAR) was funded by the National Institute of Aging to build a sustainable infrastructure and community of researchers to continue exploring older adult emergency care.
References
- Singal BM, Hedges JR, Rousseau EW, et al. Geriatric patient emergency visits. Part I: Comparison of visits by geriatric and younger patients. Ann Emerg Med. 1992;21(7):802-807.
- Hedges JR, Singal BM, Rousseau EW, et al. Geriatric patient emergency visits. Part II: Perceptions of visits by geriatric and younger patients. Ann Emerg Med. 1992;21(7):808-813.
- Baraff LJ, Bernstein E, Bradley K, et al. Perceptions of emergency care by the elderly: results of multicenter focus group interviews. Ann Emerg Med. 1992;21(7):814-818.
- McNamara RM, Rousseau EW, Sanders AB. Geriatric emergency medicine: a survey of practicing emergency physicians. Ann Emerg Med. 1992;21(7):796-801.
- Jones JS, Rousseau EW, Schropp MA, Sanders AB. Geriatric training in emergency medicine residency programs. Ann Emerg Med. 1992;21(7):825-829.
- Strange GR, Chen EH, Sanders AB. Use of emergency departments by elderly patients: projections from a multicenter data base. Ann Emerg Med. 1992;21(7):819-824.
- Rosen T, Shah M, Lundebjerg NE, et al. Impact of Jahnigen/GEMSSTAR Scholarships on Careers of Recipients in Emergency Medicine and on Development of Geriatric Emergency Medicine. Acad Emerg Med. 2018;25(8):911-920.
- Terrell KM, Hustey FM, Hwang U, Gerson LW, Wenger NS, Miller DK. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16(5):441-449.
- Carpenter CR, Gerson LW. Geriatric Emergency Medicine. In: LoCicero J, R.A. R, Katlic MR, Pompei P, eds. A Supplement to New Frontiers in Geriatrics Research: An Agenda for Surgical and Related Medical Specialties. New York City: American Geriatrics Society; 2007:45-71.
- Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci. 2011;66(7):775-783.
- Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17(3):316-324.
- Snider T, Melady D, Costa AP. A national survey of Canadian emergency medicine residents’ comfort with geriatric emergency medicine. CJEM. 2017;19(1):9-17.
- Hogan TM, Olade TO, Carpenter CR. A profile of acute care in an aging America: snowball sample identification and characterization of United States geriatric emergency departments in 2013. Acad Emerg Med. 2013;21(3):337-346.
- Schumacher JG, Hirshon JM, Magidson P, Chrisman M, Hogan T. Tracking the Rise of Geriatric Emergency Departments in the United States. J Appl Gerontol. 2018 (in press);24.
- Sanders AB. Emergency Care of the Elder Person. St. Louis MO: Beverly Cracom Publications; 1996.
- Meldon SW, Ma OJ, Woolard R. Geriatric Emergency Medicine. New York: McGraw Hill; 2004.
- Kahn JH, Magauran BG, Olshaker JS. Geriatric Emergency Medicine: Principles and Practice. Cambridge United Kingdom: Cambridge University Press; 2014.
- Murdoch I, Turin S, Johnston B, MacLullich A, Losman E. Geriatric Emergencies. West Sussex, United Kingdom: Wiley Blackwell; 2015.
- Mattu A, Grossman SA, Rosen PL, et al. Geriatric Emergencies: A Discussion-Based Review. West Sussex United Kingdom: Wiley Blackwell; 2016.
- Carpenter CR, Stern M, Sanders AB. Caring for the Elderly. In: Rowe BH, Lang ES, Brown MD, Houry D, Newman DH, Wyer PC, eds. Evidence-Based Emergency Care. Oxford United Kingdom: Wiley Blackwell; 2009:260-270.
- Hwang U, Carpenter CR. The Geriatric Emergency Department. In: Wiler JL, Pines JM, Ward MJ, eds. Value and Quality Innovations in Acute and Emergency Care. Cambridge United Kingdom: Cambridge University Press; 2017:82-90.
- Carpenter CR, Taleghani N. Older Adults in the Wilderness. In: Auerbach PS, Cushing TA, Harris NS, eds. Auerbach’s Wilderness Medicine. Vol 2. 7th ed. Philadelphia PA: Elsevier:2149-2164.
- Hwang U, Morrison RS. The geriatric emergency department. J Am Geriatr Soc. 2007;55(11):1873-1876.
- Rosenberg M, Carpenter CR, Bromley M, et al. Geriatric Emergency Department Guidelines. Ann Emerg Med. 2014;63(5):e7-e25.
- Ellis B, Carpenter CR, Lowthian J, Mooijaart S, Nickel C, Melady D. Statement on Minimum Standards for the Care of Older People in Emergency Departments by the Geriatric Emergency Medicine Special Interest Group of the International Federation for Emergency Medicine. CJEM. 2018;20(3):368-369.
- Stevens M, Hastings SN, Markland AD, et al. Enhancing Quality of Provider Practices for Older Adults in the Emergency Department (EQUiPPED). J Am Geriatr Soc. 2017;65(7):1609-1614.
- Moss JM, Bryan WE, Wilkerson LM, et al. An Interdisciplinary Academic Detailing Approach to Decrease Inappropriate Medication Prescribing by Physician Residents for Older Veterans Treated in the Emergency Department. J Pharm Pract. 2019;32(2):167-174.
- Dresden SM, Hwang U, Garrido MM, et al. Geriatric Emergency Department Innovations: The Impact of Transitional Care Nurses on 30-day Readmissions for Older Adults. Acad Emerg Med. 2019 (in press).
- Biese KJ, Busby-Whitehead J, Cai J, et al. Telephone Follow-Up for Older Adults Discharged to Home from the Emergency Department: A Pragmatic Randomized Controlled Trial. J Am Geriatr Soc. 2018;66(3):452-458.
- Hwang U, Hastings SN, Ramos K. Improving Emergency Department Discharge Care with Telephone Follow-Up. Does It Connect? J Am Geriatr Soc. 2018;66(3):436-438.
- Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med. 2015;22(1):1-21.
About the Author

