St. Joseph’s University Medical Center
Jennifer Leaman, RN, MBA, Chelsea Dehn, RN, and Tony Rosen, MD
St. Joseph’s University Medical Center (SJMC) is a large, urban academic hospital located in the midsize city of Paterson, New Jersey (population approximately 150,000) with a catchment area that includes the city and surrounding suburbs. SJMC has 650 in-patient and 88 emergency department (ED) beds and an annual ED census of approximately 100,000 patients. Twelve percent of ED patients are adults aged 65 years or older. SJMC is a pioneer and national leader in geriatric emergency medicine. It has a 20-bed specialized Geriatric Emergency Department (GED)—launched more than 10 years ago—and was among the first in the US to receive Level 1 GED Accreditation through the American College of Emergency Physicians. SJMC Chief of Emergency Medicine Marianna Karounos was instrumental in initiating and supporting SJMC’s participation in the adoption and implementation of the Elder Mistreatment Emergency Department (EMED) Toolkit. Dr. Karounos is a geriatric emergency medicine expert, having led the SJMC GED since 2013. Previously, she had completed a Geriatric Emergency Medicine fellowship at Weill Cornell Medicine, working closely with National Collaboratory to Address Elder Mistreatment core faculty; this relationship fostered her interest in joining the National Collaboratory to test the feasibility of implementing the newly developed EMED Toolkit. Additionally, Dr. Karounos and the SJMC ED team recognized they were likely missing cases of elder mistreatment and were unsure how to optimally approach intervention and management once identified.
Addressing Elder Mistreatment Prior to Toolkit Implementation
As part of their large GED, SJMC has two dedicated geriatric nurse navigators who comprehensively assess older adult patients and assist with disposition and care transitions. If an ED nurse was concerned that the patient they were seeing was experiencing elder mistreatment or had other social needs at discharge, they engaged these geriatric nurse navigators. If appropriate, the geriatric nurse navigators reported to Adult Protective Services (APS) and/or referred the patient to other appropriate community-based organizations.
Prior to EMED Toolkit deployment, the geriatric nurse navigators had pre-established relationships with APS and the New Jersey Aging and Disability Resource Connection. However, ED staff seldom identified or reported elder mistreatment, and elder abuse screening was not routinely conducted initially at triage or later during the ED visit. Therefore, identification relied on the clinical suspicion of the ED team or geriatric nurse navigator during their evaluation. Prior to implementation, ED staff completed the Emergency Department Assessment Profile (EM-EDAP) to identify gaps in elder mistreatment care at SJMC. Nearly half (48%) of active SJMC ED staff completed the EM-EDAP, with respondents including medical (55% of all respondents), nursing (42%), and administrative (3%) team members. Notably, more than half (63%) of respondents reported having received formal education or training on elder mistreatment detection, management, or reporting. All respondents who had not received any training reported interest in receiving it. Most respondents reported feeling confident in their ability to recognize, intervene, and report cases of elder mistreatment, yet only one out of eight staff reported that they often recognize cases of elder mistreatment. Additionally, only 19% of medical staff and 33% of nursing staff reported feeling more than somewhat knowledgeable about best practices in managing mistreatment cases. Notably, SJMC ED staff reported that the top three barriers to addressing elder mistreatment in the ED are lack of time to conduct a thorough evaluation, reliance on family members or caregivers for medical and social historical information, and communication difficulties with older adults. Ranking of barriers differed among nursing and medical staff. For example, the top barrier among nursing staff was lack of time to conduct a thorough evaluation, while the top barrier among medical staff was communication difficulties with older adults.
Implementing the Toolkit to Address Elder Mistreatment
Most ED nursing staff participated in a training on how to use the new screening tool. Following EM-EDAP administration, 83% of bedside ED nurses took the 30-minute online training on how to administer the brief screen portion of the Elder Mistreatment Screening and Response Tool (EM-SART). The geriatric nurse navigators, serving as clinical champions, participated in a more extensive four-hour clinical training. These trainings improved ED staff knowledge, demonstrated by improved performance on a post-test (mean score of 5.01) vs. a pre test (mean score of 4.41). While this difference is statistically significant (p=0.05), the scores themselves are not dramatically different, perhaps because SJMC’s baseline score was relatively high (maximum possible score was 10). Despite overall improvements, knowledge gaps persisted in terms of understanding what constitutes elder mistreatment, who can report suspected cases, and the role of AP.
Bedside nurses and geriatric nurse navigators shared responsibility for screening. At SJMC, ED staff implemented the EM-SART as a two-step process. First, trained triage or bedside nurses administered a brief screen for elder mistreatment with patients aged 65 years or older. This brief screen was incorporated into the electronic medical record (EMR) as required fields to improve adherence and to make it easier for nurses to document results. In cases where the brief screen indicated potential mistreatment, the nurse notified a geriatric nurse navigator, who then conducted the full screen using a paper form. Geriatric nurse navigators bring extensive experience in geriatric emergency care and care transitions. SJMC levered this expertise by having navigators conduct the more intensive full screen, which also reduced the workload for triage and bedside nurses.
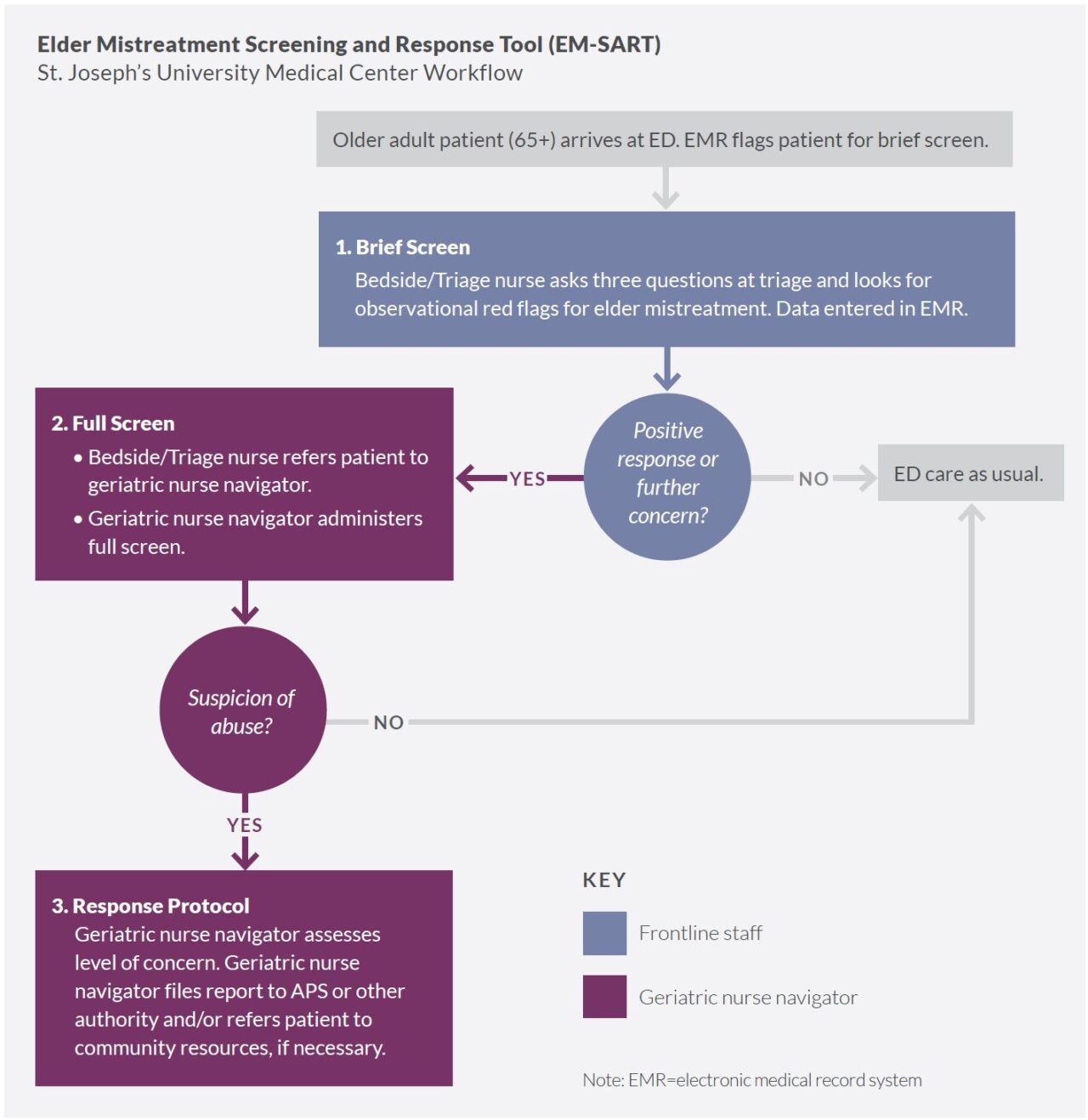
Notably, as navigators do not work the night shift, patients who received a brief screen overnight indicative of mistreatment were held in the ED until morning when one of the geriatric nurse navigators could conduct the full screen and determine the appropriate next steps.
SJMC connected with additional community partners to address elder mistreatment. Limited resources in the surrounding area reduced referral options to prevent future mistreatment. Therefore, SJMC used the Community Connections Roadmap to facilitate collaborative conversations with previously engaged stakeholder organizations to address suspected elder mistreatment: New Jersey Adult Protective Services, New Jersey Aging and Disability Resource Connection, and the Passaic County Prosecuting Attorney’s Office. They also engaged team members from the SJMC Accountable Care Organization, recognizing that this stakeholder had a financial incentive to minimize mistreatment and keep older adults at home. When considering level of service integration and network functioning on a continuum from reporting to connecting to collaborating, SJMC is categorized as being at the connecting stage, in which they are engaging community resources beyond APS, and are moving toward collaborating, in which they will formalize an elder mistreatment team.
Factors Affecting Toolkit Implementation
SJMC integrated the EM-SART brief screen into its EMR. Although still considered to be an alpha (vs. a final) version, SJMC clinical champions advocated for including the EM-SART brief screen in the EMR, with the rationale being that it would increase the likelihood of the tool’s use, and would more realistically model how the tool would be used in their ED should they continue implementation following the testing period. Integrating the EM-SART into the ED workflow via EMR modifications was an involved process that required significant support from SJMC’s IT team. However, the IT team was engaged in other high priority projects within the institution, and did not have immediate capacity to modify the EMR and develop code to extract data for reporting on this new information. Therefore, EM-SART deployment was delayed until the brief screen could be built into the EMR. Moreover, when the brief screen was initially added to the EMR, the system neither required nursing staff to administer the brief screen nor enter data collected, so key information was infrequently included. In response, the SJMC team worked with IT to create fields requiring tool administration and data entry. While these modifications dramatically improved adherence, nurses did not enter information into the EMR in a standardized fashion. Subsequently, analysis of screening data proved challenging.
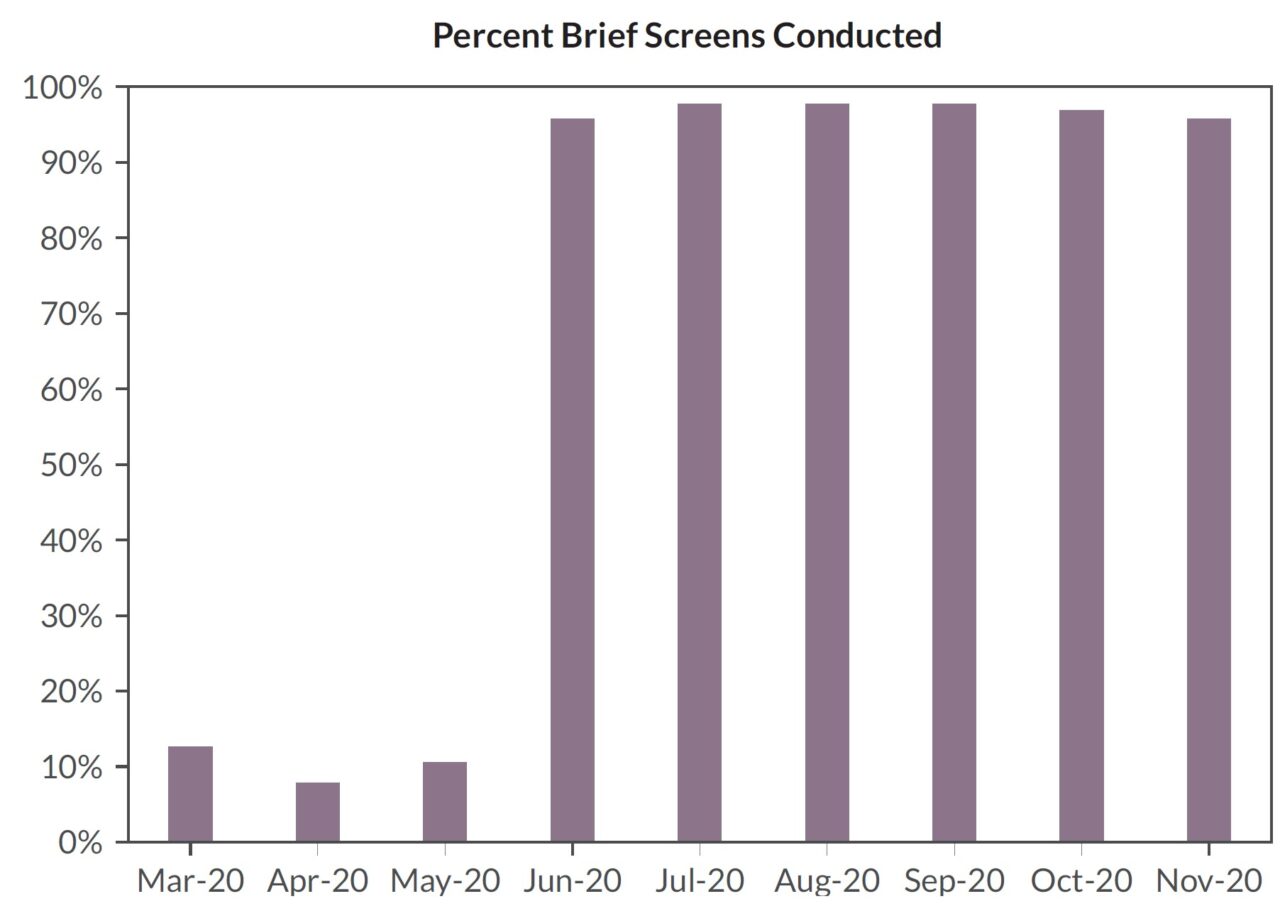
SJMC temporarily paused Toolkit implementation in Spring 2020. SJMC was deeply impacted during the initial COVID-19 surge in Spring 2020. ED resources were totally overwhelmed in caring for critically ill patients, including residents of several large local nursing homes. Few older adults from the community presented to the ED during this period, partly because of concern of COVID-19 exposure. Many ED and leadership staff became ill with COVID-19 and/or were required to quarantine or isolate, making staffing the ED very challenging. IT support had to devote all available resources to modify the EMR and generate reports related to managing COVID-19.
SJMC geriatric nurse navigators brought specialized knowledge and skills. Having geriatric nurse navigators on staff serving as clinical champions and administering more intensive full screening of patients identified at risk helped facilitate model implementation. In hospitals like SJMC that employ this type of nursing model, geriatric nurse navigators focus on issues affecting older patients that require more attention, due to their specialized expertise in health issues and care specific to older adults. This allows general nursing staff more availability to continue meeting with and assessing other ED patients. Further, having access to the resources of SJMC’s Level 1 Accredited Geriatric Emergency Department and the institution’s experience implementing other geriatric protocols made implementation of this program easier.
Results of Implementation
ED-based elder mistreatment screening, identification, and response increased over the implementation period. SJMC was able to administer the brief screen with a majority (5,648 patients, 59%) of ED patients aged 65 or older. Notably, during the initial COVID-19 surge (March – May 2020), with no requirement to enter brief screen data into the EMR, ED nursing staff performed the brief screen on an average of only 10% of eligible ED patients. In the subsequent months (June – November 2020), the brief screening rate dramatically increased to an average of 97% of eligible ED patients. This suggests that after the COVID-19 surge, with a requirement to enter brief screen data in place, ED staff were able to successfully integrate the brief screen into their workflow. During the nine-month implementation period, 85 brief screens indicated potential elder mistreatment (1.5% positivity rate). Notably, in 74 (87%) of the positive brief screens, a SJMC geriatric nurse navigator did not conduct a follow-up full screen, suggesting that either bedside nurses did not communicate the results of the screen to a geriatric nurse navigator or that SJMC staff relied on information other than the brief screen outcome to determine which cases did or did not require a more intensive screen. Alternatively, geriatric nurse navigators or other SJMC staff may have conducted components of the full screen without documenting their findings. Still, based on the results of the brief and subsequent full screens, geriatric nurse navigators identified 11 older adults as victims of elder mistreatment, with 10 receiving referrals to APS and/or law enforcement.
Few modifications were made to the implementation protocol. As mentioned above, the requirement to enter brief screen data into the EMR was the key modification to the protocol that impacted screening rates. This requirement led to a dramatic improvement in the percentage of patients receiving the brief screen. While adding a screening requirement in an EMR system may produce a higher rate of patients screened, it does not necessarily yield accurate assessments. As SJMC staff noted, EMR-embedded screens sometimes create the temptation for busy nurses to “click through,” entering data without actually asking the patient the screening questions. Issues with fidelity of ED screening are well-described, particularly for questions that seldom yield affirmative responses. Also, though required by the EMR to enter information about the brief screen, nurses did not enter information in a standardized fashion, making analysis of results difficult. For example, the EMR included the option for the nurse to indicate that the patient was not screened (for a variety of reasons), and some nurses checked this option, but others did not.
ED staff knowledge, attitudes, and practices improved. Compared to other hospital EDs participating in the EMED Toolkit’s feasibility test, implementation at SJMC was not associated with relatively large positive changes in staff knowledge, attitudes, and practices regarding elder mistreatment. EM-EDAP data collected before and 12 months after EMED Toolkit initiation showed that a greater proportion of respondents reported that they agreed that medical staff are prepared to recognize (83% at Time 2 v. 71% at Time 1) and intervene (82% at Time 2 v. 64% at Time 1) in suspected cases of elder mistreatment, and that nursing staff are prepared to intervene (72% at Time 2 v. 57% at Time 1) in suspected cases of elder mistreatment. Perceptions of staff knowledge, confidence in their ability to address elder mistreatment, and attitudes and beliefs about elder mistreatment did not significantly change from what were relatively strong scores prior to Toolkit implementation. It is possible that, due to SJMC’s longtime commitment to leadership in geriatric emergency medicine, its Level 1 Accredited GED, and a team of geriatric nurse navigators supporting and training staff, many team members were already aware of elder mistreatment and its clinical importance before care model implementation. Notably, only a small percentage (16%) of active staff responded to the second EM-EDAP administration, which reduces confidence in the findings, as it is possible that those who did not respond felt differently.
In focus groups and interviews, staff reported that the care model was well-integrated into clinical practice, and building the brief screen into the EMR system was extremely helpful. Staff reported that the handoff between nurses and geriatric nurse navigators was particularly beneficial. Staff also described improvements in their ability to identify cases of suspected elder mistreatment based on the signs and symptoms they learned about in the training modules, and they reported believing that the EM-SART helped to detect potential elder mistreatment.
Toolkit implementation did not disrupt ED functions. Data on SJMC ED metrics collected during
the pre-implementation and implementation periods suggest that EMED Toolkit implementation did not appear to have a significant negative impact on ED functions. Mean length of stay varied substantially within the pre-implementation and implementation periods—likely due to treatment of different volumes of patients with COVID-19—but did not differ significantly between pre-implementation and implementation. Percentage of older adults admitted to the hospital (59% pre-implementation vs. 42% during implementation) and 30-day returns to the ED (35% vs. 22%) were lower during the implementation period, suggesting that the care model did not have an adverse impact on ED functioning. Notably, though, the ED identified only 11 patients as victims of mistreatment, so changes noted in these metrics would have been more likely attributable to the impact of other factors, including the COVID-19 surge.
Key Lessons Learned
SJMC demonstrated that the care model may be implemented in a highly resourced large urban academic hospital ED with a GED and specialized geriatric nurse navigators. It is possible to incorporate the brief screen into the EMR and to screen a large percentage of older adult patients. Integrating existing specialized resources strengthens the care model. Incorporating the process into ED workflow did not have a measurable negative impact on ED operations.
This implementation highlighted key issues for future dissemination as well. Clearly, integrating the brief screen tool into the EMR is helpful both in ensuring that the screen is completed for patients as well as for tracking and reporting purposes. While SJMC only included the brief screen in the EMR, it is likely optimal to also build in the full screen. This way, when a brief screen is positive, the EMR can automatically pull up the follow-up screen and ensure that it is completed, thereby more comprehensively tracking screening behaviors and outcomes in the ED. However, SJMC’s experience integrating the EM-SART brief screen into the EMR proved challenging, and entering screening data into the EMR likely needs to be required in the system or it will seldom be completed. Designing and implementing changes to the EMR can vary widely in complexity, but in most cases, engagement from the IT support team is critical both before and after deployment given the challenges involved in integrating the screening tool into the EMR, existing workflows, and analyzing screening data. Further, additional training is needed for ED staff on standard data entry practices; otherwise, different providers may approach data entry differently, making subsequent care model analysis and quality improvement challenging.
In many cases, SJMC staff did not follow the EMED Toolkit’s two-step screening protocol, and did not conduct—or at least document—the full screen after a positive brief screen. Presumably, the triage or bedside nurse conducting the initial screen, or the geriatric nurse navigator receiving the handoff, used clinical judgement to determine that, despite potentially suggestive responses or observations on the brief screen, mistreatment was very unlikely. It is also possible that the triage or bedside nurse did not notify the geriatric nurse navigator about a positive brief screen, highlighting the potential importance of a flag within the EMR or another strategy to make sure that this handoff between staff is completed. Regardless, not conducting the full screen potentially represents a missed opportunity to identify elder mistreatment and initiate intervention. Since similar issues will likely occur at other sites implementing this care model, strategies for future dissemination involving implementation recommendations, training, and benchmarking should be developed.
Follow-up and the Future
SJMC ED staff have continued to routinely assess for elder mistreatment using the EM-SART. The screening remains mandatory in the EMR, with handoff to the geriatric nurse navigators if concern is identified. One of the clinical champions has since taken a new position on the in-patient hospital units at SJMC and is interested in incorporating elements of the care model in these units
“The program has improved health practices in such a way that we are aware that elder mistreatment is . . . something that we need to look at, at all times . . . It’s the same as, I need to do a CPR . . . So [this new care model] really helps us, the nurses, to be aware of it and to make sure that we are identifying this type of mistreatment in our elderly population. So, it really helps us [with] awareness“
–SJMC ED staff member
About the National Collaboratory to Address Elder Mistreatment and EDC
With funding from The John A. Hartford Foundation and the Gordon and Betty Moore Foundation, the National Collaboratory to Address Elder Mistreatment was founded in 2016 with a charge to develop a scalable response to the prevalence of elder mistreatment. This group is comprised of national experts in elder mistreatment from the University of Southern California Keck School of Medicine, University of Massachusetts Medical School, the University of Texas Health Science Center at Houston, and Joan & Sanford I. Weill Medical College of Cornell University, with Education Development Center (EDC) serving as the Collaboratory convener, EDC is a global nonprofit with more than 60 years experience designing, testing, and implementing innovative programs addressing critical challenges in health, education, and economic inequality.
To learn more: contact us at NCEAEM@edc.org or visit https://www.edc.org/national-collaboratory-address-elder-mistreatment