Lyndon B. Johnson Hospital
Jason Burnett, PhD, and Sherry Plummer, MSN, RN
Lyndon B. Johnson Hospital (LBJ), part of the Harris Health System, operates the busiest Level III trauma center and emergency department (ED) in Texas. It receives over 80,000 patient visits per year, with approximately 10% of these patients aged 65 years or older. The hospital’s catchment area includes the two communities in Harris County with the highest rates of referrals to Adult Protective Services (APS). This fact, along with Harris Health System’s commitment to quality care, encouraged the LBJ leadership team, the ED Social Work Case Management leadership team, and frontline ED staff to join the National Collaboratory to Address Elder Mistreatment’s efforts to stem the tide of elder mistreatment. In addition, Dr. Carmel B. Dyer, a leading expert in elder mistreatment prevention and management based at LBJ, championed efforts to work with the National Collaboratory to test the feasibility of implementing the Elder Mistreatment Emergency Department (EMED) Toolkit.
Addressing Elder Mistreatment Prior to Toolkit Implementation
LBJ ED staff includes physicians; triage, bedside, charge, and forensic nurses (i.e., sexual assault nurse examiners); and social work case managers. Prior to EMED Toolkit implementation, nurses conducted sporadic and unsystematic screening for elder mistreatment, consulting with physicians and/or Social Work Case Management at will for related physical exams and discharge planning. The standard discharge practice consisted of providing the patient with a list of community resources, available in both English and Spanish. However, staff did not verify that the contact information included on the handout was correct, or that the organizations listed were still providing services. Additionally, ED staff did not follow up to determine if the patient contacted the resource(s) and received services.
Between July and September 2019, 39% of active ED staff responded to the Elder Mistreatment Emergency Department Assessment Profile (EM-EDAP), providing a clear picture of perceived needs to improve their response to potential cases of elder mistreatment. Less than half (40%) of respondents reported having received formal education or training on elder mistreatment detection, management, or reporting. Most (89%) of the respondents who had not received such training reported interest in receiving it. Staff most frequently referenced lack of education on addressing elder mistreatment as the most pressing issue that they faced when caring for older adults who have been mistreated. Although over half of respondents reported feeling confident in their abilities to recognize, intervene, and report cases of elder mistreatment, most (73%) staff also reported that they sometimes or often miss cases of elder mistreatment. Additionally, only 5% of medical staff, 25% of nursing staff, and 42% of other staff reported feeling very knowledgeable about best practices in managing mistreatment cases. ED staff reported that the top three barriers to addressing elder mistreatment in the ED were lack of specialized community services for older adults vulnerable to mistreatment, lack of time to conduct a thorough evaluation given competing priorities with other patients, and reliance on family members or caregivers for medical and social history. Nursing staff ranked lack of specialized community services and lack of time to conduct
a thorough evaluation equally as the top barrier, while medical staff ranked lack of specialized community services as the top barrier.
Implementing the Toolkit to Address Elder Mistreatment
Specialized and bedside nurses, as well as social workers, completed relevant training on how to use the new screening tool. From October through December 2019, 55% of bedside nursing staff completed a 30-minute online training on administering the brief screen portion of the Elder Mistreatment Screening and Response Tool (EM-SART), 75% of charge nurses and ED managers completed the training on administering the full screen portion of the EM-SART, and 100% of social worker case managers and clinical nurse case managers completed the four-hour onsite clinical training on all topics related to implementing the new tool. Brief screen trainings resulted in improved knowledge, demonstrated by improved performance on a brief screen training post-test (mean score of 5.04) vs. a pre-test (mean score of 4.52). Despite the improved scores, concerns remained about which caregiver behaviors indicated elder mistreatment, the responsible agent for conducting the physical exam, and red flags for unsafe discharge.
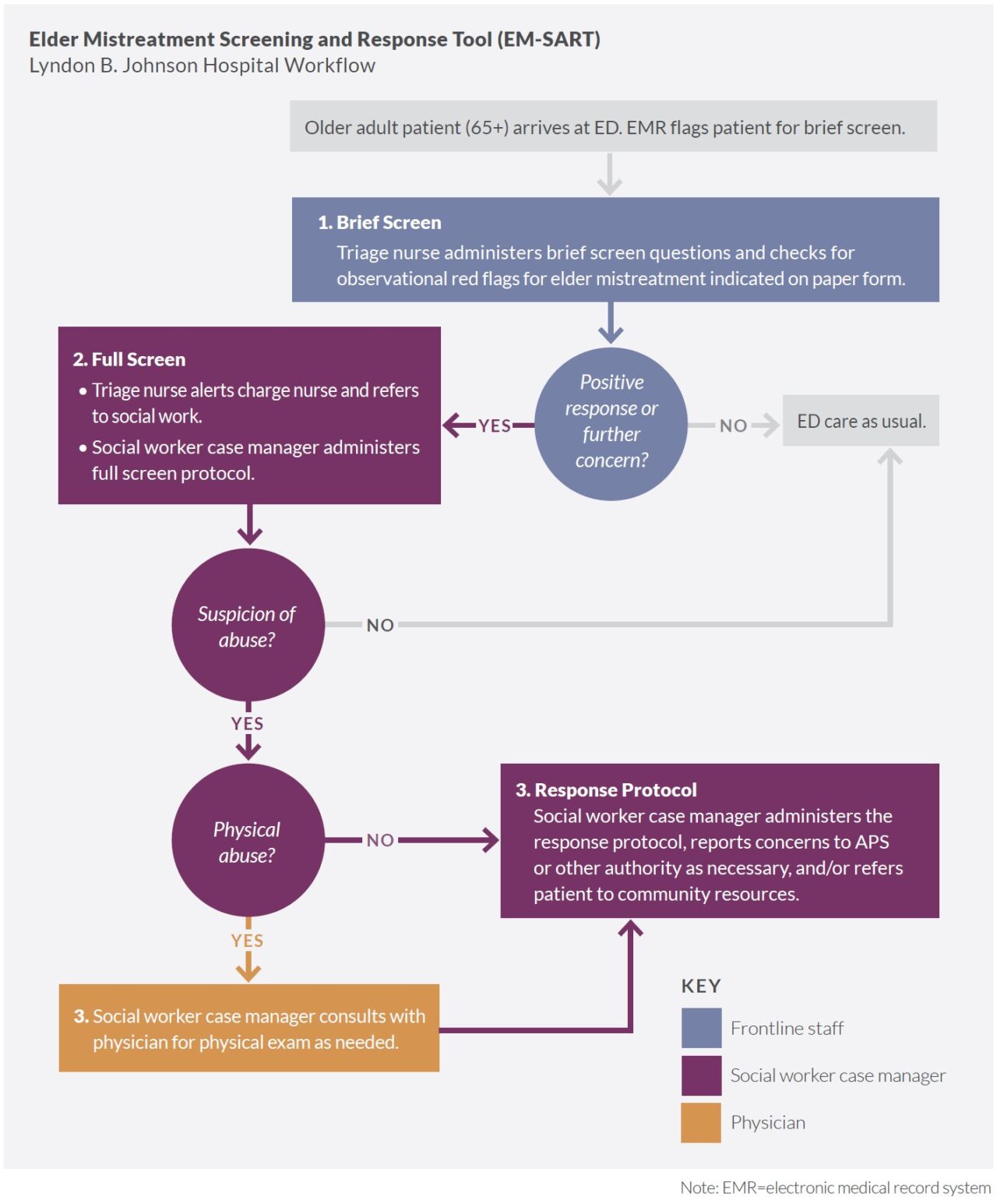
Bedside nurses, charge nurses, and social workers shared responsibility for screening. LBJ ED staff implemented the EM-SART between January and December 2020 as a three-step process. First, triage or bedside nurses administered the brief screen to adults aged 65 years or older presenting in the ED and notified a charge nurse when a screen was positive. The charge nurse then prompted a social worker case manager to complete a more in-depth assessment (or full screen) that included a physician consultation when screening indicated potential physical abuse. When a full screen indicated suspicion of elder mistreatment, the social worker completed a subsequent APS report and connected the patient to community resources.
Social workers reported suspected cases of elder mistreatment to APS. LBJ did not use the Community Connections Roadmap to advance connections with and further engage surrounding community resources to address elder mistreatment during the feasibility study. ED Social Work Case Management staff had a good working relationship with APS and were reporting suspected cases of elder mistreatment to appropriate authorities. When considering level of service integration and network functioning on a continuum from reporting to connecting to collaborating, LBJ is categorized as being at the reporting stage and is moving toward the connecting stage in which they will be engaging more community resources beyond APS.
Factors Affecting Toolkit Implementation
LBJ, like other hospitals participating in the feasibility study, faced many challenges during the EMED Toolkit implementation phase. The EMED Toolkit feasibility test began on the heels of a Centers for Medicare & Medicaid Services (CMS) medical review—a process that takes precedence over new initiatives. Additionally, LBJ experienced a significant fire and flood that displaced hospital staff and limited building accessibility and services. High nursing turnover rates made retaining dedicated and trained personnel a challenge. Last, but not least, the COVID-19 pandemic required rapid cycle changes by hospital staff to ensure both patient and employee safety. Observing caregiver interactions as indicated in the EM-SART was not possible in the COVID-19 setting. These challenges made even the slightest shift in screening onerous. Still, ED staff demonstrated resilience when facing these challenges, citing several facilitating factors: the streamlined screening process, pre-established close working relationships between nursing and social work staff, and the availability of 24-hour social work assistance.
Results of Implementation
LBJ modified the brief screen tool and implementation process. In May 2020, LBJ added several observational items to the EM-SART brief screen at the request of ED social workers to ensure tool sensitivity for cases that fit their patient population (i.e., those experiencing physical abuse, neglect, and financial exploitation). These observations included suspicious bruising, poor hygiene, and evidence of malnutrition, as well as indication of financial exploitation. While LBJ ED social work staff were modifying the brief screen, nursing staff began conducting the full screen. Because nurses were often holding unstructured conversations with patients when a brief screen was positive, this change led to significant reduction in the use of the formal full screen to assess and document evidence of potential mistreatment, as well as decreased data tracking for the Toolkit feasibility test.
ED-based elder mistreatment screening, identification, and response rates were sensitive to onset of COVID-19 protocols and workflow modifications. LBJ ED screening of older adults for elder mistreatment prior to EMED Toolkit implementation is unknown. During EMED Toolkit implementation, however, 1,218 brief screens (20% of ED patients aged 65 years or older) were completed, resulting in 23 positive brief screens and four full screens that prompted staff to submit reports to APS. In the four cases reported to APS, staff suspected that patients were experiencing psychological abuse, physical abuse, and neglect (physical and medical). In addition, one patient was believed to be experiencing financial exploitation in conjunction with another form of abuse. All four patients appeared to lack, or have limited access to, needed resources, and all presented with fractures, malnutrition, and dehydration. Based on the results of each full screen, staff instituted safety planning for three out of the four suspected cases. Missing full screen data for 19 of the positive brief screens may have affected the actual number of EM cases reported. Noticeable trends in both screening and positive screen rates correlated with the onset of the COVID-19 pandemic (decreased brief screening rates), nursing staff taking over administration of both the brief and full screens (increased brief screening rates and decreased full screening rates), and inclusion of additional observational items on the brief screen (increased positive brief screen rates).
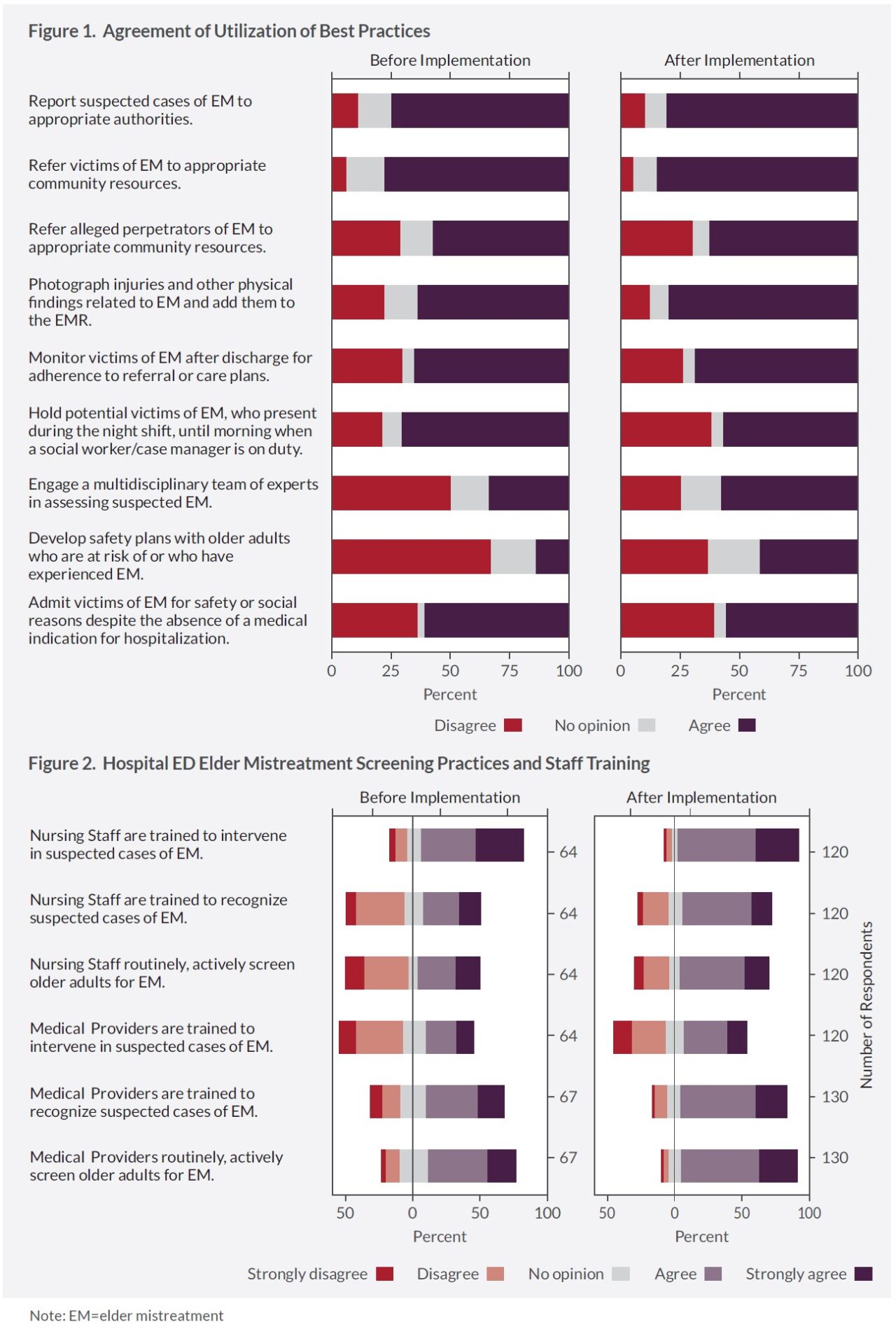
ED staff knowledge, attitudes, and practices improved. Between January and March of 2021, the second round of the EM-EDAP was administered to LBJ ED staff to assess staff profile changes regarding best practices for detecting, managing, and reporting elder mistreatment. The response rate increased from 39% to 43% and consisted of physicians and nurses only. Responses indicated that the project had led to an overall improvement in staff reported knowledge of best practices for addressing elder mistreatment. The largest positive impacts included recognition of medical and nursing staff roles in screening, developing safety plans with older adults who are at risk of or who have experienced elder mistreatment, and monitoring patients after discharge for adherence to referral or care plans.
There were slightly more modest increases in perspectives on reporting potential elder mistreatment to APS. Almost all staff reported that they believed elder mistreatment was an important public health problem warranting screening, detecting, and reporting in the ED. However, more staff reported that monitoring patients after discharge from the ED was not their responsibility. There was little change in staff perceptions on access to community resources. Staff perceive that there are few community resources available to older adults at risk of experiencing mistreatment; yet most agree that APS and law enforcement are receptive and helpful in cases of elder mistreatment.
Indicators of ED functioning during Toolkit implementation changed slightly. There were slight downward shifts in the LBJ ED median and mean lengths of stay that followed the implementation timeframe, with the highest medians and means occurring pre-implementation, followed by the implementation period and the post-implementation period, respectively. These shifts may not be operationally significant and possibly confounded by the effects that the COVID-19 pandemic had on LBJ ED operations. There were fewer older adults, and fewer patients of all ages in general, presenting in the ED during the height of the pandemic.
Within six months of EMED Toolkit implementation, staff intentions towards assessment, management, and response to elder mistreatment improved, along with an overall increased focus on older adults.
“It brings a more focused assessment based on the elderly, in addition to what we already do. So, I think it enhances our current practice. And it provides a service to patients that may otherwise fall through the cracks . . . it’s good for our patients. It’s good for our community.“
–LBJ ED staff member
Encouraging was that while the program initially seemed daunting, it was ultimately determined to be feasible following training and implementation. The protocol created a common language across frontline workers—a critical component for efficient care in the busy LBJ ED setting. At the end of the implementation period, nursing staff expressed determination to continue screening beyond the implementation phase thereby underscoring its sustainability.
Key Lessons Learned
LBJ leadership and ED staff, facing a global pandemic, fire, flooding, and a CMS audit, demonstrated their dedication and commitment to the health and safety of older adults by participating in this national project promoting screening, management, and response to elder mistreatment in the ED setting. Through training and participation in the implementation of the EMED Toolkit, staff increased their knowledge of best practices for addressing elder mistreatment and their skills in conducting brief and in-depth screening. A streamlined elder mistreatment screening process fit into ED staff’s daily workflow, resulting in over 1,200 completed assessments. During EMED Toolkit implementation, LBJ adopted a proactive response to suspicion of elder mistreatment, established a universal language regarding mistreatment, and strengthened collaboration among ED staff. Ultimately, LBJ ED and social work staff helped to create safer environments for older adults in the Harris Health System catchment area.
Still, several unmet challenges persisted during EMED Toolkit implementation. A significant proportion of ED bedside nursing staff did not complete the EM-SART training, potentially negatively affecting the screening rates. A few months into implementation, nursing staff replaced full screens with unstandardized conversations to assess the outcomes for patients with positive brief screens. When
these conversations led to determinations of suspected elder mistreatment and/or reports to APS, this information was not necessarily documented. LBJ was unable to incorporate the EM-SART into the electronic medical record system (EMR), and relied on paper screening forms for documentation, which ultimately resulted in misplaced forms and the diminished ability to track patient data. Finally, the inconsistency of discharge processes was a significant barrier to EMED Toolkit implementation, potentially due to the high turnover rates among nursing and social work staff.
Follow-up and the Future
Future implementations of the EMED Toolkit will likely benefit from having a lead ED physician on site to champion the EMED Toolkit and to mandate or promote a culture that encourages participation in training activities. The experience at LBJ shows that designating (and paying) a specific staff person to monitor EMED Toolkit implementation fidelity may increase detection and reporting of suspected elder mistreatment cases. So that other hospital EDs can implement the EMED Toolkit with greater ease, EM-SART screening modules should be integrated into the EMR to prompt complete screening and documentation and protect against lost information. Moreover, future implementation should include more discharge planning education on critical factors associated with safe discharge, alternatives to same place or unsafe discharge, methods for ensuring efficient response by appropriate agencies when discharge delays occur due to safety admissions, and ED staff awareness of potentially harmful discharge locations.
“The biggest difference is that we are intentional about seeking out versus waiting. We’re more proactive, should I say. . . with this assessment. . .”
–LBJ ED staff member
About the National Collaboratory to Address Elder Mistreatment and EDC
With funding from The John A. Hartford Foundation and the Gordon and Betty Moore Foundation, the National Collaboratory to Address Elder Mistreatment was founded in 2016 with a charge to develop a scalable response to the prevalence of elder mistreatment. This group is comprised of national experts in elder mistreatment from the University of Southern California Keck School of Medicine, University of Massachusetts Medical School, the University of Texas Health Science Center at Houston, and Joan & Sanford I. Weill Medical College of Cornell University, with Education Development Center (EDC) serving as the Collaboratory convener, EDC is a global nonprofit with more than 60 years experience designing, testing, and implementing innovative programs addressing critical challenges in health, education, and economic inequality.
To learn more: contact us at NCEAEM@edc.org or visit https://www.edc.org/national-collaboratory-address-elder-mistreatment