Eastern Niagara Hospital
Tony Rosen, MD and Heather Loftus, RN, MSN
Eastern Niagara Hospital (ENH) is a small community hospital located in Lockport, a small town in western New York State. Located about 30 miles from the city of Buffalo, it primarily serves a rural population. ENH has 134 in-patient and 8 emergency department (ED) beds and an annual ED census of approximately 14,000 patients. Thirty-two percent of ED patients are adults aged 60 years or older. ENH participated in the initial implementation of the Elder Mistreatment Emergency Department (EMED) Toolkit with support from the Health Foundation for Western and Central New York, which is committed to reducing elder mistreatment through interventions in health care. The ENH President and CEO was a supportive champion for the project, as the ENH ED team wanted to improve their care for older adults at risk of or experiencing mistreatment. They recognized that they were likely not identifying all cases of elder mistreatment and were unsure how to respond to the cases they were identifying.
Addressing Elder Mistreatment Prior to Toolkit Implementation
Prior to EMED Toolkit deployment, the ENH ED did not have a streamlined protocol in place for identifying and responding to cases of elder mistreatment. Because ENH does not have any social workers in the ED or the hospital, a nurse care manager handled case management, care coordination, and discharge planning for admitted patients. ED medical providers or nurses addressed any social needs for patients discharged from the ED, including reporting to Adult Protective Services (APS) and making referrals to community-based organizations. While Niagara County has a county-based APS and Office for the Aging, as well as a Center for Elder Law and Justice nearby in Buffalo, the ENH ED did not have a close collaborative relationship with these organizations.
To identify and address gaps in elder mistreatment and care at ENH, ED staff were invited to complete the Emergency Department Assessment Profile (EM-EDAP). Nearly half (44%) of active ENH ED staff completed the EM-EDAP. Most respondents (54%) reported never or rarely recognizing a case of elder mistreatment, and over half (64%) reported believing that they had missed cases of elder mistreatment. Only one respondent (7%) reported having received any formal training in elder mistreatment detection, intervention, or reporting. All other ENH ED staff members responding reported that they would like additional elder mistreatment education. Notably, ENH ED staff reported believing that the top three barriers to addressing elder mistreatment in the ED were: lack of a protocol for a streamlined response to elder mistreatment, lack of basic training and knowledge, and limited follow-up by protective services when cases were reported.
Implementing the Toolkit to Address Elder Mistreatment
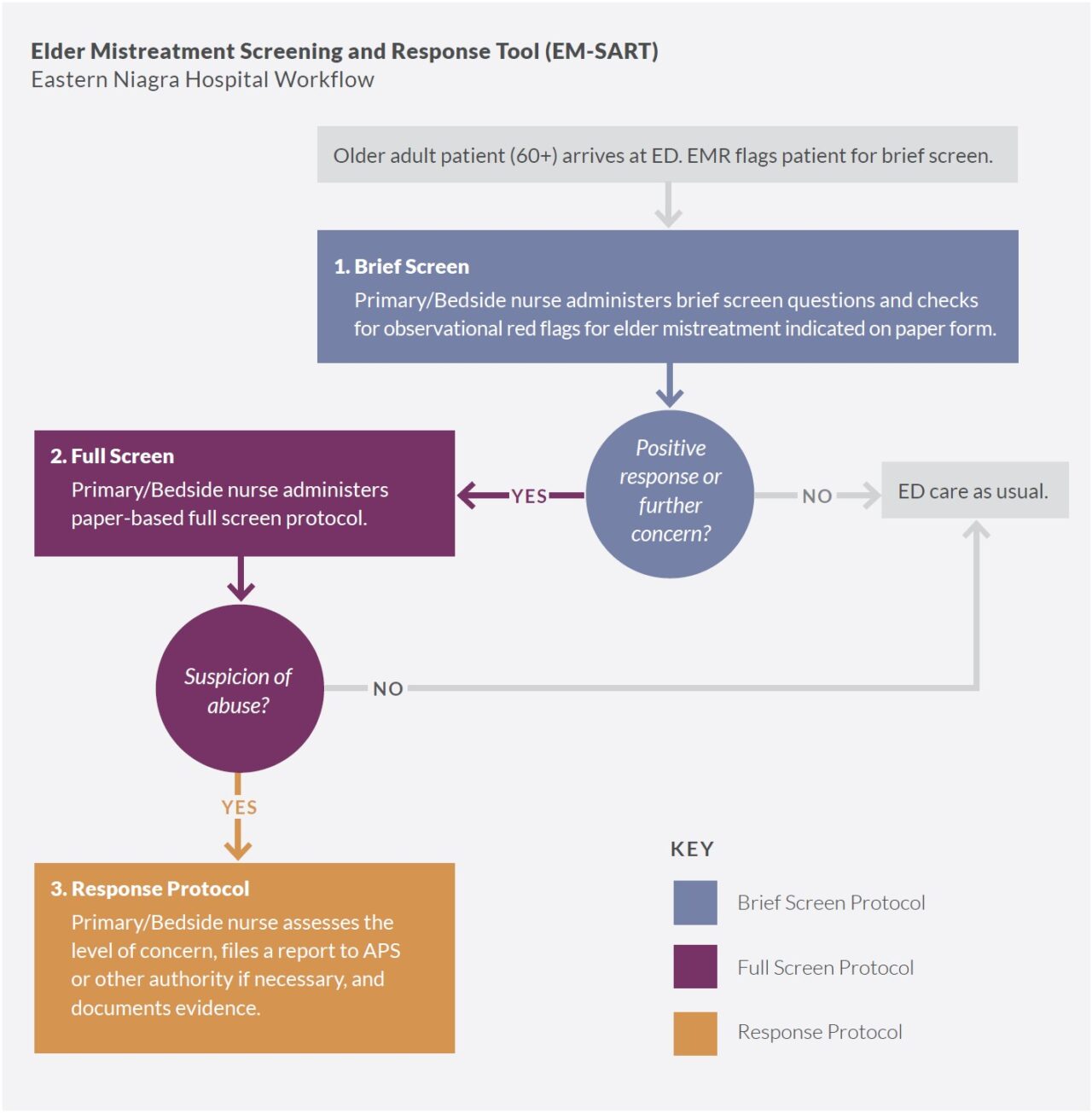
Most ED nursing staff participated in a training on how to use the new screening tool. Following EM-EDAP administration, 83% of ED nursing staff participated in an hour-long training on how to screen for elder mistreatment using the Elder Mistreatment Screening and Response Tool (EM-SART), a two-stage screening tool that includes a brief screen and a more thorough full screen followed by response protocol to be used when patients screen positive. An ED nursing leader participated in a more extensive four-hour clinical training. These trainings increased ED staff knowledge, demonstrated by improved performance on a post-test (mean score of 11.2) vs. a pre-test (mean of 10.2). Staff also reported satisfaction with both screening and response.
ED bedside nurses conducted both brief and full screens. At ENH, the primary or bedside nurse providing care to the patient implemented the entire elder mistreatment screening and response process, including the brief screen as well as the full screen, and any appropriate interventions. This workflow differed from that at other implementation sites—typically larger hospitals—where one provider conducted the brief screen during triage, then handed off patients for whom there was concern for elder mistreatment to another clinician (often a social worker or specialized geriatric care coordinator) to conduct the more in-depth assessment and response. ENH leadership acknowledged the potential value of a hand-off to a more highly trained provider after the brief screen, but given staffing levels in their small ED, the only realistic approach was to have the primary or bedside nurse conduct the entire process. Nursing staff recorded results of the screening and response process on paper forms that staff then scanned into the electronic medical record (EMR).
ENH began improving communication with APS. ENH used the Community Connections Roadmap to initiate collaborative conversations with stakeholder organizations including: Niagara County Adult Protective Services, Niagara County Office for the Aging, and the Center for Elder Law and Justice. When considering level of service integration and network functioning on a continuum from reporting to connecting to collaborating, ENH is categorized as being at the reporting stage, in which they are improving communication with APS, and is moving toward the connecting stage, in which they will engage community resources beyond APS.
Factors Affecting Toolkit Implementation
Paper screening tools were difficult to integrate into ED workflow. Integrating the EM-SART into practice was initially difficult because the tool was paper-based. ENH ED staff were accustomed to receiving prompts to enter information within the EMR, particularly with protocol changes and new initiatives. They struggled with remembering to use the paper forms, lowering screening rates. ENH leadership subsequently developed a system whereby a registration staff member handed the screening form directly to the nurse when the patient was assigned to them, making the process much smoother and more reliable.
ENH clinical champion role changed hands during implementation. Because of personnel and responsibilty changes, the clinical champion role at ENH was transferred to a new person twice during the initial implementation, which may have impacted program oversight and messaging to staff about the care model. Nevertheless, the presence of an ED nurse clinical champion and a supportive hospital administrator were critical factors in facilitating implementation.
The COVID-19 outbreak affected ED workflow and patient volumes. The initial implementation of the EMED Toolkit at ENH coincided with the beginning of the COVID-19 outbreak, which had a dramatic effect on ED workflows, resources, and patient volume. During the first months of the COVID-19 outbreak, the ENH ED had ever-changing COVID-19 protocols and was unable to devote time or resources to ensuring that the elder mistreatment care model was being deployed effectively or to troubleshooting issues with the initiative’s roll-out. Additionally, fewer older adults were seeking care in the ENH ED, given concerns about COVID-19 exposure, and the ED temporarily implemented new triage and assessment protocols, including curbside evaluation of patients in their cars. Notably, ENH, demonstrating flexibility and innovation, successfully added elder mistreatment screening to their curbside assessment.
Results of Implementation
ENH’s extensive screening of older patients for mistreatment yielded few positive cases. ENH was able to perform the brief screen on a large majority (2,679 patients, 87%) of ED patients aged 60 years or older. This rate was higher than most other implementation sites, suggesting that ED staff were able to successfully integrate this initial step into their protocols. Notably, however, only 17 brief screens were positive (0.6% positivity rate)—a rate much lower than at other sites. Despite core faculty and the ENH clinical champion exploring reasons for this and modifying the protocol, positivity rates did not increase significantly during the implementation period. Also, in 16 of the 17 brief screens that were positive (94%), the ENH ED provider did not conduct a follow-up full screen. This suggests that ENH staff relied on other information to determine that, despite positive findings on the brief screen, 16 of the 17 cases did not require a more intensive screen. Alternatively, ENH providers may have conducted components of the full screen without documenting them. During the 9-month implementation period, only one older adult was identified as a victim of elder mistreatment. This patient did not require screening but rather presented clearly as a victim of elder mistreatment, evidenced by police involvement after serious traumatic injury at the hands of a family member. Due to his injuries, he was transferred to a Level 1 trauma center for additional care, and therefore did not receive community referrals, and the case was not reported to APS.
ENH modified the brief screen to include more patient observations. During implementation, ENH employed a strategy to potentially increase positive brief screens. They adapted the brief screen to include additional patient observations (visible bruising, poor hygiene [dirty clothes, hair, or nails], malnutrition, and suspicion of financial exploitation). These changes did not lead to significant increases in positive brief screens, and ENH ED staff felt that they did not enhance the screening process. Notably, staff were skeptical that some of the observations (such as dirty fingernails) would be suggestive of elder mistreatment because, in their rural community, farmers may have dirty fingernails because of their work. Further, ENH staff expressed significant concern for over- identification of elder mistreatment using the brief screen.
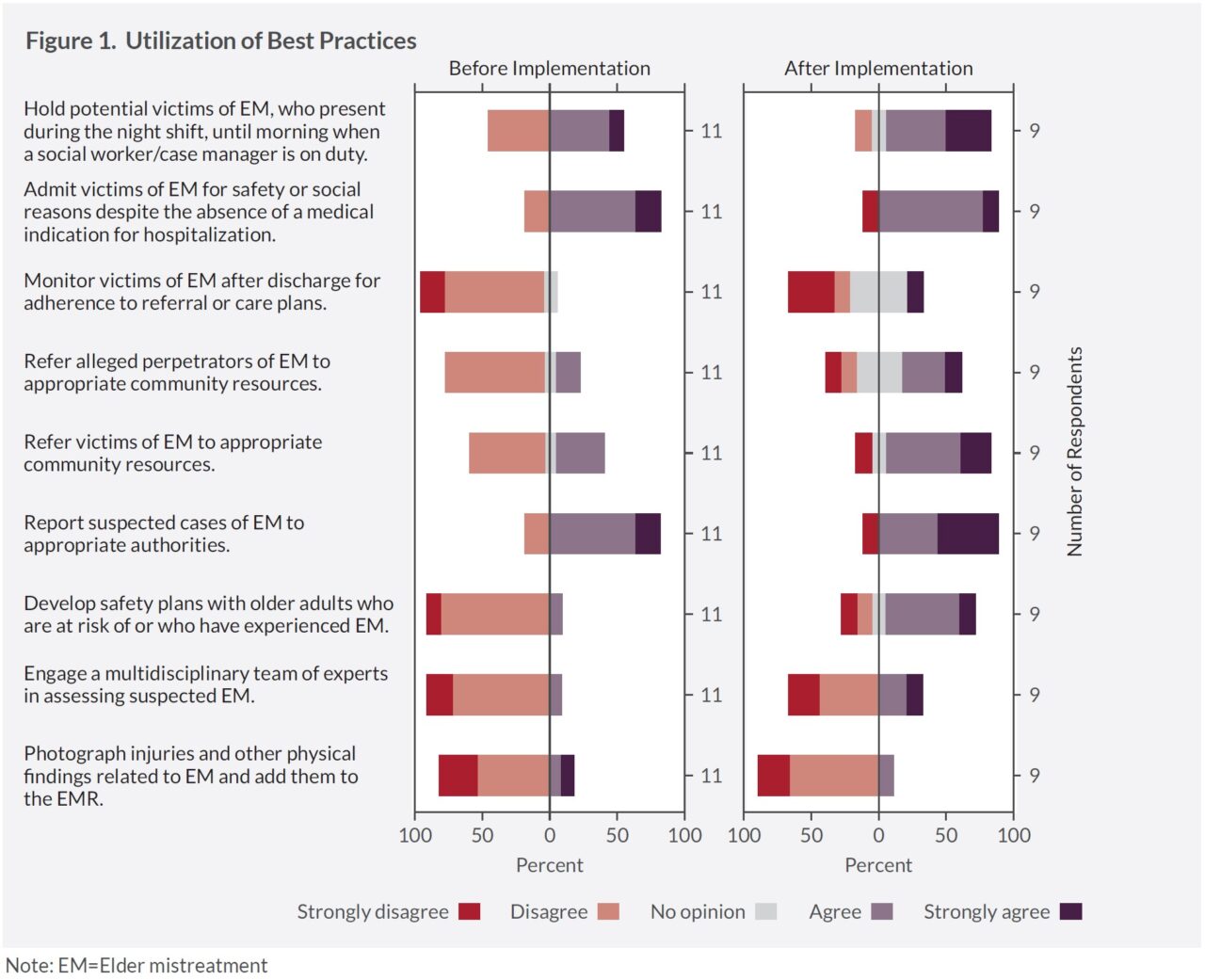
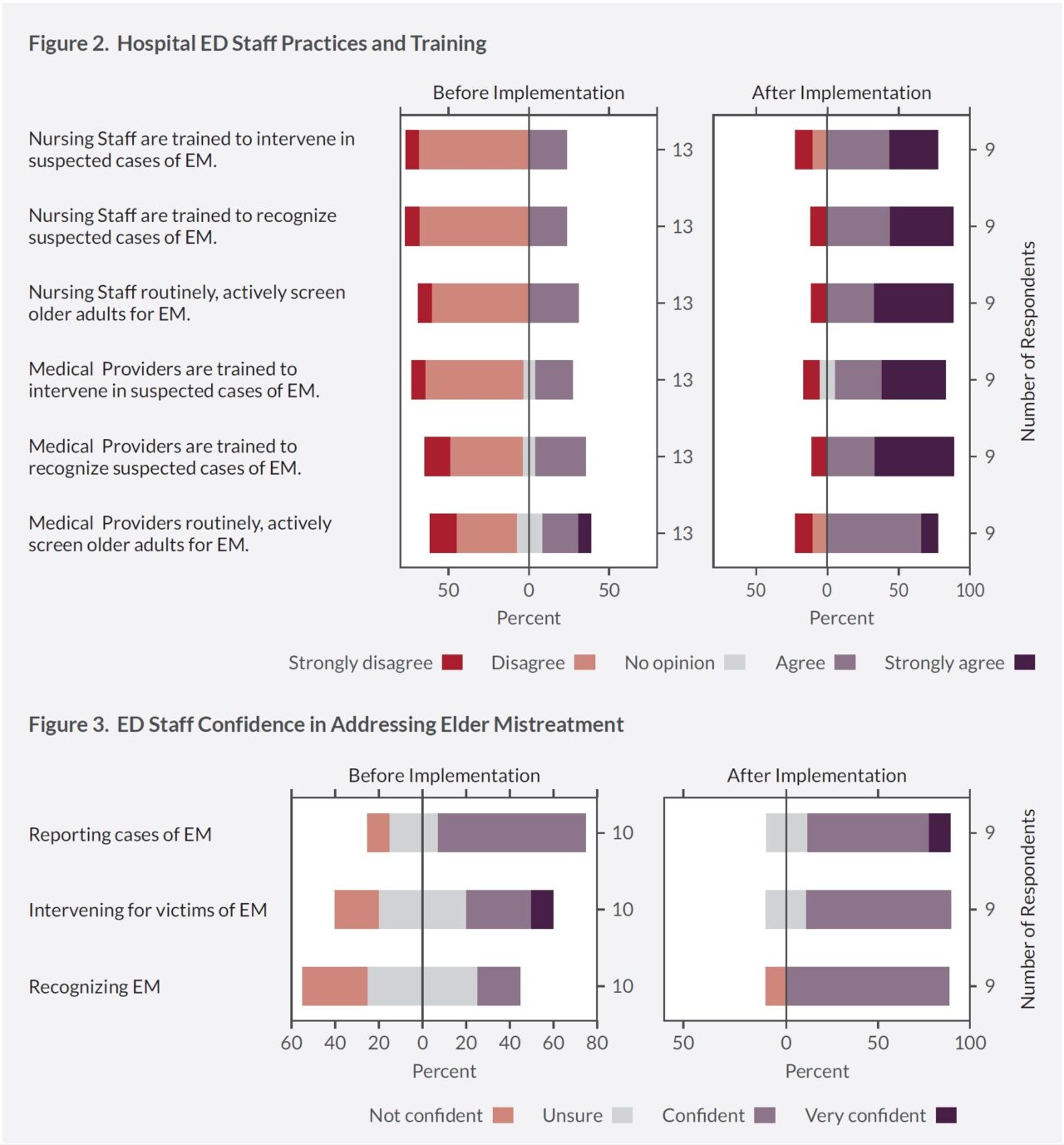
ED staff knowledge, attitudes, and practices about how to address elder mistreatment improved. Though few cases of concern were identified among older adult patients in the ENH ED, implementation of the care model had a large positive affect on staff knowledge, attitudes, and practices regarding elder mistreatment. Comparing ENH ED staff EM-EDAP results prior to and post-implementation showed several significant changes (see Figures 1, 2, and 3 below). Confidence in recognizing, responding to, and reporting elder mistreatment improved. Attitudes and beliefs about the frequency and severity of elder mistreatment, as well as the role of the ED in screening and reporting, changed. Further, ED staff reported agreeing with best practices for elder mistreatment management. Notably, ENH staff attitudes about the availability of and connections to APS and other community-based organizations did not change substantially and were less positive than at other clinical sites. This suggests an opportunity for future initiatives to connect the ENH ED to these resources more closely and effectively.
Toolkit implementation does not disrupt ED functions. A comparison of the ENH ED metrics during the pre-implementation period to the implementation period suggests that incorporating the screening process did not have a significant negative impact on ED functions. Mean and median lengths of stay were not significantly different in the pre-implementation vs. implementation periods. Further, ENH ED providers reported feeling that the screening process was not cumbersome. Percentage of older adults admitted to the hospital (27% pre-implementation vs. 25% during implementation) and 30-day returns to the ED (15% vs. 15%) also were not adversely affected, but, as the ENH ED only had a single patient identified as a victim of mistreatment, any change in these metrics would have been more likely attributable to other factors. Notably, comparing the pre-implementation to the implementation period is complicated by the outbreak of COVID-19, which coincided with the initial implementation of the care model at ENH. ED usage was impacted dramatically by COVID-19, with the number of overall visits dropping sharply and lengths of stay minimized in efforts to avoid exposure.
Key Lessons Learned
ENH demonstrated that the care model may be implemented in a small community hospital ED serving rural areas with limited specialty staff. It is possible to screen a large percentage of older adult patients and the model is acceptable to ED staff. Incorporating the care model into the ED workflow has a positive impact on knowledge, attitudes, and practices among ED staff about elder mistreatment, an important but underappreciated phenomenon.
An examination of this implementation reveals significant concerns about the care model, however, that have implications for future dissemination. Despite a high rate of performance of brief screening, the care model did not identify cases of elder mistreatment in the ENH ED, and therefore did not significantly impact care for older adult patients during the implementation period. The rate of positive brief screens was much lower than at other clinical sites, and most positive brief screens did not result in the completion of a full screen. There are many potential factors that contributed to the very low rate of positive brief screens. It is possible that nurses conducted the screening in a public, rather than private, setting with the potential for the abuser to be present. Nurses may have asked the questions as part of other routine ED screens before a rapport had been created to facilitate disclosure. If busy, nurses may have completed the paper form without actually asking the patient the screening questions. Issues with fidelity of ED screening are well-described, particularly for questions that seldom yield affirmative responses. Nurses may not have asked the questions of older adults with dementing illness, presuming that they were unable to report accurately, despite research that suggests they can. Additionally, having the primary/bedside nurse conduct both the brief screen and the full screen may have created perverse incentives. In the ENH workflow, rather than a hand-off to a specialized provider, a positive brief screen led to more work for the nurse to explore in greater detail whether the older adult was truly a victim. In addition to being time-consuming, the full screen includes questions that the nurse may find uncomfortable to ask or potentially stigmatizing to the patient. This may have encouraged the nurse to interpret unclear or borderline brief screen results as negative.
Further, we found that ENH staff were concerned about over-identification of potential elder mistreatment, such as misinterpretation of the patient’s unkempt appearance, and may have preferred to err on not pursuing elder mistreatment, particularly in patients with an acute medical issue that was unrelated. It is also possible that patients served by ENH are less likely to become victims of elder mistreatment and/or less willing to divulge their victimization to ED providers than in other communities. This seems unlikely to be a significant contributor, though, as previous research has suggested that elder mistreatment is present in all communities. Also, other clinical sites with similar catchment area population demographics identified many more cases. Additionally, ENH seldom followed the care model’s two-step screening protocol, not conducting—or at least not documenting—the completion of a full screen after a positive brief screen. Presumably, they used clinical judgement in these cases to determine that, despite potentially suggestive responses or observations on the brief screen, mistreatment was very unlikely. In addition, they may have thought that it was only important to identify elder mistreatment among community-dwelling older adults, presuming that patients coming from nursing homes were safe/low risk even if the brief screen was positive. Not conducting the full screen, though, potentially represents a missed opportunity to identify elder mistreatment and initiate intervention. Similar issues will likely occur at other sites implementing this care model. Strategies to address them will be developed through training, recommendations, benchmarking, and supporting clinical champions.
Follow-up and the Future
ENH ED staff have continued to routinely assess for elder mistreatment. They have, however, abandoned the paper forms, which were not always easy to use. They have emphasized the value of integrating the care model, particularly the screening component, into the EMR as a way to ensure that it remains part of the ED workflow. ENH has been purchased by Catholic Health, which is constructing a new hospital called Lockport Memorial, a campus of Mt. Saint Mary’s Hospital. This state-of-the-art hospital facility is scheduled to open in 2023 and will replace ENH. The Catholic Health acquisition also anticipates a change in EMR to Epic and the health system has plans to implement the EMED Toolkit at the new hospital.
“I think it makes people look at their practice in a different way and allows them to identify [signs of abuse] that maybe would have gone by the wayside when it’s not quite so straightforward.”
–ENH ED staff member
About the National Collaboratory to Address Elder Mistreatment and EDC
With funding from The John A. Hartford Foundation and the Gordon and Betty Moore Foundation, the National Collaboratory to Address Elder Mistreatment was founded in 2016 with a charge to develop a scalable response to the prevalence of elder mistreatment. This group is comprised of national experts in elder mistreatment from the University of Southern California Keck School of Medicine, University of Massachusetts Medical School, the University of Texas Health Science Center at Houston, and Joan & Sanford I. Weill Medical College of Cornell University, with Education Development Center (EDC) serving as the Collaboratory convener, EDC is a global nonprofit with more than 60 years experience designing, testing, and implementing innovative programs addressing critical challenges in health, education, and economic inequality.
To learn more: contact us at NCEAEM@edc.org or visit https://www.edc.org/national-collaboratory-address-elder-mistreatment