About UNC Hillsborough Level II GED
A community hospital in Hillsborough, NC with a 15-bed Emergency Department.
- 26,000 annual ED visits
- 4,500 visits per year for those over 65
- It serves as an extension of the UNC Medical Center and is staffed by the same pool of providers.
- Not-for-profit institution
- In 2023, 2,086 unique ACO beneficiaries visited UNC Hillsborough Level II GED 3,441 times, resulting in a cost of $5,926,177 for the associated payor.
About UNC Senior Alliance
UNC Senior Alliance is a division within the UNC Health Alliance, UNC Health’s physician-led clinically integrated network and population health services organization.
- UNC Senior Alliance partners with the Centers for Medicare and Medicaid Services (CMS) to participate in their innovative alternative payment models, a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. UNC Senior Alliance participated in the Next Generation ACO model from 2017 through 2021. Today, UNC Senior Alliance is participating in the Medicare Shared Savings Program (MSSP ACO).
- In 2023, UNC Senior Alliance beneficiaries visited a GED 4,931 times, representing 22% of total ED visits.
Background
UNC Hillsborough Level II GED and the UNC Senior Alliance were invited to participate in West Health Institute’s (WHI) Learning and Action Network (LAN), connecting value-based care organizations (VBCOs) to Geriatric Emergency Departments (GEDs). West Health’s LAN model borrows from the Institute for Healthcare Improvement’s Model for Improvement, which focuses on utilizing Plan-Do-Study-Act (PDSA) cycles to drive incremental and data-driven improvements.
Motivation
The partnership between the UNC Senior Alliance and UNC Hillsborough was mutually beneficial because it had the potential to impact a high-risk population that frequently utilizes ED services. The partnership allowed for novel cross-collaboration by bringing together different stakeholders in value-based care and care delivery. Both groups of stakeholders were committed to rerouting patients to higher-value care pathways through existing referral pathways and clinical infrastructure. Both sets of stakeholders wanted to serve the older adult population better while promising to provide more cost-effective care, streamline workflows, and improve hospital throughput. Participating in the larger West Health LAN with other health systems provided an opportunity to learn best practices from innovative efforts nationwide.
The Partnership
Dr. Tony Rodriguez, MD, the Medical Director of Population Management at the UNC Health Alliance, partnered with Dr. Katie Davenport, MD, a geriatric fellowship-trained ED physician and Medical Director of UNC Hillsborough. Executive Sponsors, data analysts, project management, and a quality improvement coach supported this “dyad” partnership. Through this partnership, the Emergency Department became a crucial leverage point in the UNC Health system, bridging the gap between ambulatory care and acute interventions. Dr. Rodriguez reflected on this partnership by explaining that “an ED visit used to be thought of as a system failure since a patient being seen there represented a breakdown in preventative care or proper management of chronic conditions. However, we’re now seeing an ED visit as a valuable opportunity to transform a patient’s care trajectory that can lead to system-wide improvements and more efficient resource allocation.”
Goals
Overall, the goal of the LAN was to reduce avoidable admissions from the GED, resulting in gross service savings.
Problem Statement
The referral and scheduling processes for transitioning patients from the Emergency Department (ED) to ambulatory clinics were complex and inconsistent, varying significantly across different specialty clinics. Each clinic had built its own referral process in isolation, so when the project started, there was no system-level integration. This lack of standardization created confusion for ED providers and led to delays in patient care. Communication gaps between the ED and speciality clinics resulted in missed opportunities for timely follow-ups and coordinated care. Additionally, providers faced challenges in scheduling appointments due to limited visibility into clinic availability, and the absence of a robust referral tracking system hindered the ability to measure outcomes and ensure patients received necessary follow-ups.
The Improvement Initiative
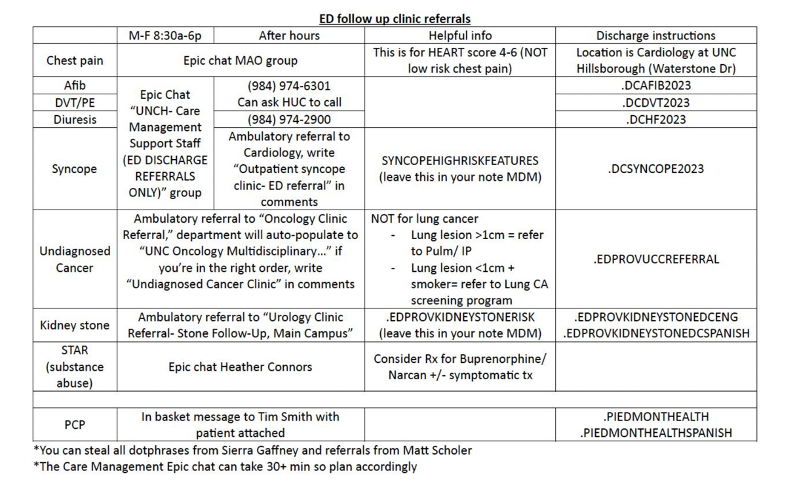
The improvement initiative focused on streamlining referral and scheduling processes for the included clinics: DVT Clinic, A-Fib Clinic, IV Diuresis Clinic, Syncope Clinic, and Chest Pain Clinic. These clinics were selected due to their involvement in managing subacute conditions that could prevent avoidable hospital admissions and ED visits. Specific process inefficiencies were identified, and solutions were designed to improve referral rates, reduce provider burden, and improve patient outcomes. Below are several PDSA cycles that were implemented during the solutions-based approach:
- Outsourcing scheduling responsibility to Care Manager Assistants
This PDSA cycle focused on transitioning scheduling responsibilities from ED providers to a Care Manager Assistant (CMA), working to streamline the referral process. This change aimed to reduce the burden on providers, who previously managed to schedule phone calls themselves, often resulting in delays and confusion. A full-time team of CMAs was introduced to manage referrals during business hours, improving reliability and efficiency.
- Provider Feedback
A pre/post provider satisfaction survey was implemented via Qualtrics to evaluate the impact of the new referral and scheduling workflow. The pre-survey, conducted in September 2023, revealed gaps in provider awareness (70%) and satisfaction (49%) with the existing scheduling process. Providers described the prior method as confusing and cumbersome, with feedback highlighting the need for a centralized resource for scheduling. After five months of the Care Management Pathway, the follow-up survey in March 2024 showed significant improvements: awareness increased to 84%, and satisfaction rose to 80%.
- Engaging the Patient’s Voice
The patient voice was incorporated to evaluate the referral process from a patient-centered perspective. Leveraging existing geriatric nurse callbacks, targeted questions were added to assess patient experiences, follow-up success, and comfort with outpatient transitions. Of those surveyed, 67% reported positive experiences with their transition clinic appointments, and 81% did follow up as scheduled.
Challenges
The improvement initiative faced a few technical and logistical challenges. First, it became quickly apparent that GED clinicians required the use of the established alternative pathways 24/7/365, despite the outpatient clinics operating on a normal schedule. This posed a scheduling problem and the UNC team worked closely with the Care Management team to ensure that any pending requests that came in overnight would be addressed the next business day. Second, tracking referrals to clinics was not a function embedded within the EHR, so the project team had to track ad hoc EPIC secure chat messages manually. During the year-long LAN, UNC worked with its internal technical teams to begin building a more official, streamlined, and robust EHR referral pathway but faced numerous delays along the way. Finally, educating GED clinicians about the availability of the outpatient clinics (Fig. 1) as a disposition option resulted in capacity challenges within a few of the specialty clinics. Capacity challenges were not anticipated, and those clinics quickly became inundated with patients, leading to longer wait times. As a result, UNC began working with their GED clinicians and outpatient clinics to further triage and prioritize outpatient referral based on greatest need.
Results
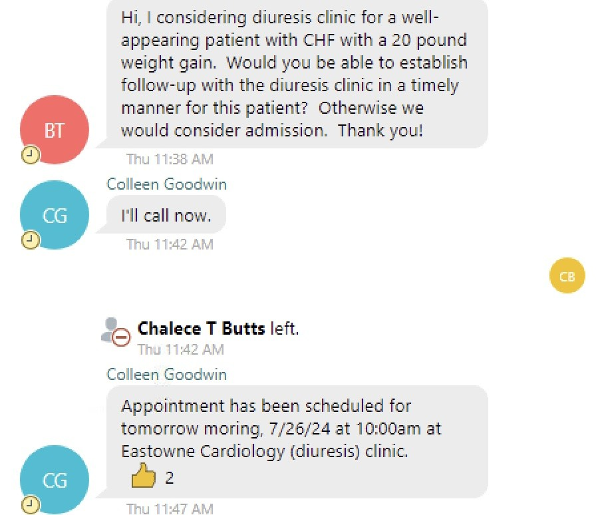
Connecting rapid, out-patient, specialty care services into Level II GED disposition options resulted in 146 averted admissions and $2,046,628 in gross service savings, from January 1, 2024 to September 30, 2024. More importantly, 146 older adults were able to receive care more aligned with their goals and what matters most to them. Below, find an example of an EPIC secure chat in which the established process worked flawlessly to prevent an admission:
Future Goals
The results of the pilot improvement initiative were so promising that the focus shifted from completing the initial pilot to validating the financial modeling and proof of concept, which laid the groundwork for broader institutional support in UNC Health Alliance’s Strategic Plan: Forward Together 2030. As a result, UNC Health Alliance committed to a larger-scale implementation by planning to scale the referral pathways to other hospitals (UNC Rex, Chatham, Chapel Hill), addressing systemic needs rather than a narrow technical fix. This pivot represents a valuable outcome, as it aligns with UNC Health Alliance’s broader goal of creating sustainable solutions that elevate geriatric emergency care at a healthcare system level while also reducing costs to the payor and generating shared savings for the Senior Alliance.
If you are interested in learning more about how UNC Hillsborough and the UNC Senior Alliance averted 146 admissions by connecting rapid, out-patient, specialty care services into Level II GED disposition options please contact Alex Ostberg at: aostberg@email.unc.edu.