As of January 2025, hospitals in the United States are required to attest to their processes for trying to limit ED total length of stay (LOS) to under 8 hours, and time to admission to within 3 hours of the decision to admit for older adults.
A system-wide problem
Boarding is the practice of holding patients in the emergency department (ED) while awaiting an inpatient bed. It exacerbates ED crowding and decreases quality of care. ED length of stay (LOS) and ED boarding time have both increased from 2017 to 2024. A fact that should come as no surprise if you work in an ED.
Boarding is a system-wide problem. Hospital closures, staffing shortages, reduction in numbers of staffed beds, and staffing shortages in post-acute care facilities all contribute to full inpatient census. . This, in turn, increases ED boarding as patients requiring admission await a bed.
In general ED overcrowding due to boarding has been linked to delays in medication administration, lower adherence to sepsis care guidelines, longer time to antibiotic administration, delayed time to catheterization in myocardial infarction, and longer hospital length of stay. For critically ill patients, boarding in the ED is associated with longer duration of mechanical ventilation and higher overall mortality.
Harms to older adults
Geriatric patients suffer disproportionately from boarding. They are more likely to experience ED boarding while awaiting an inpatient bed. And while in the ED, they are at greater risk for negative health outcomes such as delirium or functional decline. The ED environment is associated with common contributors to delirium such as disruption of the sleep/wake cycle and sleep deprivation, dehydration, immobility, noise, and bright lights. Older adults who need assistance with activities of daily living (ADLs) who spend the night in the ED waiting for hospital admission are at greater risk of in-hospital mortality.
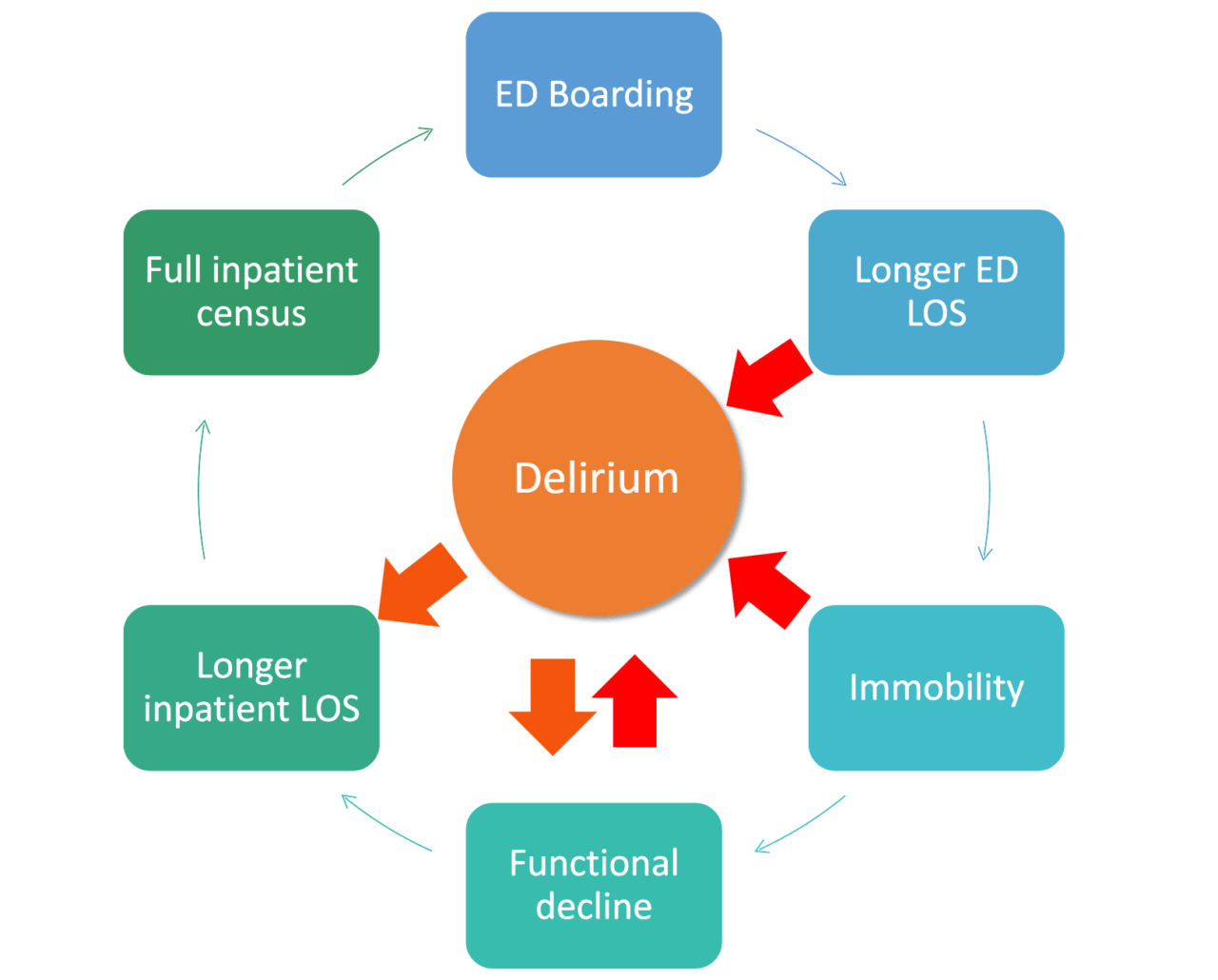
Vicious cycle of boarding
The diagram below shows how boarding leads to more boarding. When an older adult visits the ED, their risk of developing delirium increases. In patients with cognitive impairment, the risk is twofold. The emergency department is just one part of a larger system with multiple factors that lead to boarding. And if an older adult spends prolonged time boarding, they are more likely to develop delirium and then more likely to experience a longer hospital length of stay, which contributes to the vicious cycle of having to board the next patient needing an inpatient bed in the ED.
So, knowing that it’s a problem that can snowball onto itself, how can hospitals and health systems address the issue at multiple points?
Strategies for Reducing Boarding
Addressing boarding can have a multi-pronged benefits. If we can reduce ED boarding, we may see improvements in quality of care and patient outcomes, better operational throughput, shorter LOS, improved hospital capacity, better patient experience, greater staff satisfaction, and lower MD burnout.
Strategies that have been shown to improve ED boarding, reduce inpatient LOS, and improve patient outcomes include:
- Moving boarding patients from ED to inpatient hallways. The ED is deliriogenic, especially for older adults and those with underlying cognitive impairment. When hospitals moved boarding patients to inpatient hallways, it reduced inpatient length of stay and adverse patient outcomes. It was also preferred by patients.
- Smoothing elective admissions throughout the week to ensure some beds are available for patients arriving in the ED who require admission.
- Reducing delays for inpatient discharge. By making beds available earlier, hospitals can address ED buildup of patients and get the highest-risk patients into a bed sooner. Doing discharge rounds in the morning, introducing discharge lounges, and doing discharges over the weekend are just some strategies to reduce delays and free up inpatient beds.
- Enacting surge protocols when a critical threshold capacity is reached.
Reducing the Harms of Boarding (when boarding can’t be avoided)
Prioritizing Patients for ED or Inpatient Beds
For a more detailed look at creating care processes and implementing strategies for reducing harm, see our article Designing Care Processes to Reduce Boarding and Associated Harm.
In an ideal situation, your hospital could use age (65+) as a criterion for prioritization for ED room placement or admission. But in so many hospitals, the number of older adults in the ED is so large this isn’t possible. If that’s the case in your ED, consider this three-tiered approach. Prioritize patients based on:
- Risk of Harm from Prolonged Boarding: The highest risk patients are those who are frail, have a physical disability, or have underlying cognitive impairment. All these factors lead to a higher risk of developing delirium while in the ED.
- Care needs difficult to be met in the ED: This is more subjective and should be defined with the help of nursing leadership.
- Care needs not able to be met in the ED: This will be hospital-specific. Some procedures cannot be done in the ED (for example, chemotherapy initiation cannot be done in the author’s ED) therefore prioritized bed assignment is critical.
This three-tier approach can be applied to all people entering the ED. Older adults are at greater risk for frailty and cognitive impairment, but risk of delirium applies to anyone with underlying CI. So this model should capture both at-risk older adults and other at-risk patients.
Optimizing Care of Older Adults Boarding in the ED
Three aspects of care should be optimized to reduce harm to older adults boarding in the ED. These are the progression of care, normalization of function, and environment.
In a lower resource approach, your hospital could look at utilizing existing resources to address the three aspects:
- Progression of care: Standing orders for acute medic actions and ensuring home medications are continued, while ordering anticipated inpatient tests and consults to avoid lengthy waits.
- Normalization of function: regular rounding for toileting needs, ambulation protocols, meals/hydration, addressing hearing and visual impairment, normalizing sleep/wake cycle and ensuring cognitive engagement.
- Environment: put at-risk patients in their own room or in a quiet area. Turn down lights at night and reduce as much ambient noise as possible.
Where resources are available, hospitals can assign care of boarding patients to inpatient staff. This could include MDs, RNs, pharmacists, PT and OT, and other members of the interdisciplinary team. This approach has been shown to decrease hospital length of stay and mortality.
Another approach is to have a boarding unit within the ED with dedicated, specialized staff. This model has been shown to improve patient experience and outcomes.
