Polypharmacy and High-risk Medications in Older Veterans Presenting for Emergency Care
Volume 2 | Issue 12 | Article 3 - Original Research
Download PDFBackground
Patients age 60 and older represented 20% of Emergency Department (ED) visits between 2014 and 2017.1 Within the Veterans Affairs Health Care System (VAHCS), 49% of patients presenting to the ED were age 65 and older in 2019.2 Older adults often have more prescription medications and increased medical complexity.3 One study suggests that at least 39% of patients over the age of 65 years are prescribed at least 5 medications, and that overall number of prescribed medications increases with age.4 Although 5 or more medications is the most cited definition, polypharmacy has been described ranging from 2 to 11 or more medications.5 Specific medication classes that increase the risk of harm or falls in older adults include antiarrhythmics, anticholinergics, anticoagulants, anticonvulsants, antidepressants, antihyperglycemics, antihypertensives, antipsychotics, anxiolytics, opioids, sedatives, and skeletal muscle relaxants.6,7 In addition, over 50% of older adults have been prescribed at least one medication that is potentially inappropriate.8
Comprehensive medication reviews (CMRs) may reduce all-cause mortality, potentially inappropriate medications, and overall cost.9 The American College of Emergency Physicians suggest screening for polypharmacy and documentation of high-risk medications in the ED.6 The purpose of this quality improvement initiative was to describe high-risk medications and polypharmacy in older Veterans presenting to the ED in order to inform the workflow of a Geriatric ED pharmacist.
Methods
A retrospective chart review was conducted at a single, tertiary care VAHCS between 10/1/2017 and 9/30/2019. Adults aged 65 years or older who presented to the ED were included. The primary endpoint was the percentage of patients with the presence of at least one high-risk medication on the outpatient medication list.7 Secondary endpoints were the percentage of patients with at least five and ten scheduled medications, the mean number of scheduled medications per patient, and the percentage of patients on each high-risk medication class presenting to the ED. In addition, the percentage of patients on at least 5 medications or a high-risk medication and the percentage of patients 75 years or older and on at least 10 scheduled medications or a high-risk medication were evaluated. Endpoints did not include medications prescribed in the ED and included outpatient medication prescribing at presentation to the ED to expand upon previous data.10
Results
Of 63,653 patients presenting to the ED during the specified timeframe, 27,018 patients were included in the analysis (Table 1). For the primary endpoint, 22,639 (83%) patients had at least one high-risk medication on the outpatient medication list. Approximately 20,755 (76.8%) patients were found to have at least five scheduled medications, with 15,308 (56.7%) patients having ten or more medications. The average number of scheduled outpatient medications per patient was 13 ± 7. The three most common high-risk drug classes were antihypertensives (73.8%), antidepressants (40.2%), and opioids (37.8%). Overall identification of high risk-medications was similar across age groups (Figure 1). However, those over 85 years of age had less frequent prescribing of anticholinergics, anticonvulsants, antihyperglycemics, opioids, and skeletal muscle relaxants. A total of 8,464 (31.3%) patients were 75 years of age or older and on at least ten medications or one high-risk medication.
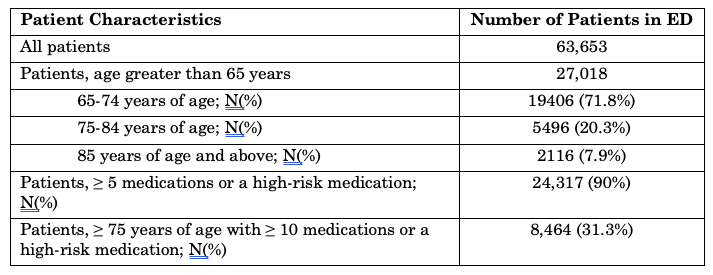 Table 1: Patient Characteristics and High-risk Medications of Older Veterans Presenting to the Emergency Department
Table 1: Patient Characteristics and High-risk Medications of Older Veterans Presenting to the Emergency Department
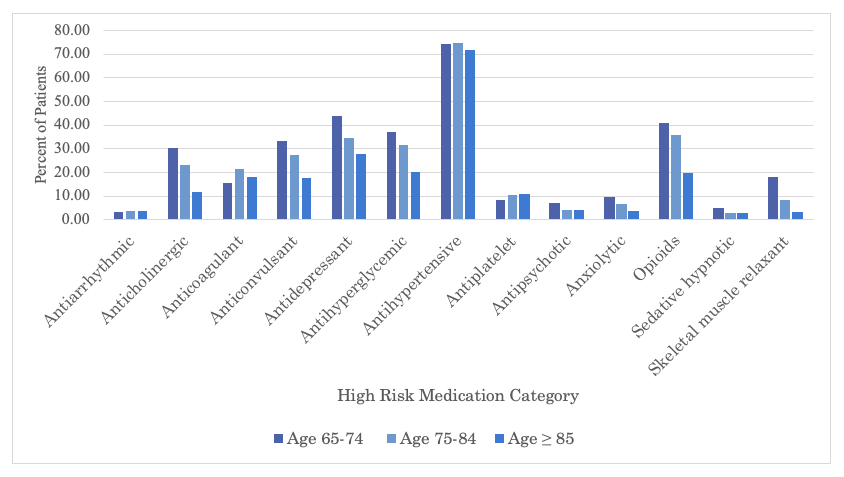 Figure 1: High-Risk Medication Classes of Older Veterans Presenting to the Emergency Department
Figure 1: High-Risk Medication Classes of Older Veterans Presenting to the Emergency Department
Discussion
Most patients were within the age range of 65 to 74 years, with less than one-third of patients over 75 years of age. We identified higher than expected rates of high-risk medication use as 83% were on at least one high-risk medication compared to 50% noted in a prior study.8 High rates of polypharmacy were also above expected with over 70% of patients on at least 5 medications compared to 40% found in a prior study.4 These higher rates may be due to the relative increased incidence of comorbid conditions and clinical complexity seen in the Veteran population. In addition, patients who require emergency care may have conditions predisposing them to high-risk medication use beyond the average primary care patient. In general, the VA population includes older patients compared to a non-VA setting, therefore this increases the likelihood of comorbidities and potential for medication prescribing. Most patients were 65 to 74 years of age, and this aligns with the general age breakdown of the VA population.11
Outside of antihypertensives, opioids and antidepressants were the second and third most frequently prescribed high-risk medications in this patient population, respectively. These medication classes may increase the risk of central nervous system-related side effects and falls.7 The higher rates of these medication classes compared to other classes may be attributed to a higher burden of mental health conditions and/or concomitant pain found within the veteran population and therefore a greater likelihood of these medication classes being prescribed.12 This also provides an opportunity for future research to further evaluate and identify additional strategies to limit need for widespread use of these drug classes. Moreover, the rate of prescribing these medication classes did appear to decrease with age potentially indicating deprescribing in the oldest cohort of patients.
Following this pilot initiative, the facility’s ED has become an identification point for geriatric patients at elevated risk of adverse events. Patients in the ED greater than 75 years of age and on at least 10 scheduled medications or a high-risk medication are currently being targeted for medication review by the ED pharmacist. A CMR is conducted that includes deprescribing recommendations to outpatient providers.
Medication management and deprescribing in the geriatric population is multifaceted and this quality improvement project focused on an intervention at the point of acute care access. Other factors are also involved in a geriatric ED setting regarding medication principles. There is a need for continued provider education regarding tapering and discontinuation of high-risk medications in older adults, in addition to caregiver and patient education.
In conclusion, 76.8% of geriatric patients presenting to the ED had at least 5 scheduled outpatient medications; 83% were on at least one high-risk medication. Screening criteria was developed for CMRs to be completed by a clinical pharmacist in the ED. Evaluation of the impact of the pharmacist intervention is an area of future development. Continued efforts toward deprescribing of high-risk medications and minimizing polypharmacy in older Veterans is also needed.
Key Words
Polypharmacy, high-risk medications, geriatric pharmacy, geriatric emergency medicine
Affiliations
Page L. Morizio PharmD BCPS1, 2, Vinita M. Mistry PharmD1, 2, Ashley E. McKnight PharmD BCPS1, Marc J. Pepin PharmD BCPS BCGP1, 2, William E. Bryan PharmD BCPS1, 2, Ryan K. Owenby PharmD1, Laura A. Previll MD MPH1-3, Luna C. Ragsdale MD MPH1, 3
- Durham Veterans Affairs Health Care System, Durham, NC
- Durham Veterans Affairs Geriatric Research Education and Clinical Center (GRECC), Durham, NC
- Duke University Hospital, Durham, NC
Conflicts of Interest
The authors have no conflicts of interest to report.
Acknowledgements
There is no funding to report.
References
- Ashman JJ, Schappert SM, and Santo L. Emergency department visits among adults aged 60 and over: United States, 2014–2017. NCHS Data Brief, no 367. Hyattsville, MD: National Center for Health Statistics. 2020. https://www.cdc.gov/nchs/products/databriefs/db367.htm. Accessed October 15th, 2021.
- Emergency Medicine Management Tool Age Report January 1, 2019 through December 31, 2019. VHA Support Service Central Capital Assets (VSSC) Dashboard. Accessed October 15th, 2021.
- Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780-791. doi:10.1111/j.1532-5415.2007.01156.x
- Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988-2010. J Gerontol A Biol Sci Med Sci. 2015;70(8):989-995. doi:10.1093/gerona/glv01
- Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. doi:10.1186/s12877-017-0621-2.
- Geriatric Emergency Department Guidelines Task Force. American College of Emergency Physicians Policy Statement: geriatric emergency department January 2019. https://www.acep.org/globalassets/new-pdfs/policy-statements/geriatric-emergency-department-guidelines.pdf. Accessed October 15th, 2021.
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-694. doi: 10.1111/jgs.15767.
- Reeve E, Bell JS, Hilmer SN. Barriers to optimising prescribing and deprescribing in older adults with dementia: a narrative review. Curr Clin Pharmacol. 2015;10(3):168-177.
- Bloomfield H, Linsky A, Bolduc J, Greer N, Naidl T, Vardeny O, et al. Deprescribing for Older Veterans: A Systematic Review. Washington, DC: Evidence Synthesis Program, Health Services Research and Development Service, Office of Research and Development, Department of Veterans Affairs. VA ESP Project #09-009; 2019. Available at: https://www.hsrd.research.va.gov/publications/esp/deprescribing-sr.pdf.
- Stevens MB, Hastings SN, Powers J, Vandenberg AE, Echt KV, Bryan WE, et al. Enhancing the Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department (EQUiPPED): Preliminary Results from Enhancing Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department, a Novel Multicomponent Interdisciplinary Quality Improvement Initiative. J Am Geriatr Soc. 2015;63(5):1025-1029. doi: 10.1111/jgs.13404.
- Veteran Population. National Center for Veterans Analysis and Statistics. https://www.va.gov/vetdata/. Accessed October 15th, 2021.
- Olenick M, Flowers M, Diaz VJ. US veterans and their unique issues: enhancing health care professional awareness. Adv Med Educ Pract. 2015;6:635-639. doi:10.2147/AMEP.S89479.