Are Geriatric Screening Tools Too Time Consuming for the Emergency Department? A Workflow Time Study
Volume 2 | Issue 6 | Quality Improvement
Full TextBox 1: Abstract
Background
The Geriatric Emergency Department (ED) Guidelines recommend that all older patients be screened for geriatric syndromes such as delirium, fall risk, frailty, and cognitive impairment. ED nurses were educated to perform three geriatric screening tools: the Delirium Triage Screen (DTS), the 4 Stage Balance Test (4SBT), and the Identifying Seniors at Risk (ISAR). We conducted a workflow time study to examine potential barriers to geriatric screening.
Methods
A standardized observational protocol was developed to assess timing, procedures, and interruptions in an academic tertiary care referral ED. Nurses caring for a patient ≥65 years old were asked to perform the screening assessments within view of the observer. Data points included starting and stopping times (measured via stopwatch) for each assessment, getting the patient out of bed for the 4SBT, and documentation. We also noted any interruptions or barriers to performing the assessments.
Results
Data were collected for 30 observations of 27 nurses. The complete geriatric screening took 177±71 (mean±SD) seconds [range 69-297] with the ISAR taking the longest to perform. The BDTS took 14±15 seconds [range 5-76] to complete. The time to stand the patient for the 4SBT was 20±27 seconds and the 4SBT took 58±28 seconds [range 6-142]. The ISAR took 81±40 seconds [range 36-216]. Interruptions occurred in three observations and were all patient questions. The majority of nurses (24/30) documented concurrently while doing the assessments. In 22 observations, ED physicians/advanced practice practitioners were unaware of how to locate the screening results in the electronic medical record.
Conclusions
Performing three geriatric screening tools took approximately three minutes of real clinical time. Performing these screenings is feasible in a busy ED setting. Physician barriers identified included accessing the results and applying the information.
Introduction
Older adults make up 15% or more of patients seen in the Emergency Department (ED) and older patients have unique needs.1 The Geriatric Emergency Department Guidelines2 recommend that all older adults be screened for geriatric syndromes in order to detect patients who may need additional resources to assist with their care. One of the difficulties of screening for any syndrome in the ED setting is the fast-paced, high-acuity, rapid-workflow culture of the ED.3 Previously researched barriers to ED screening include the time needed for completion, the need for additional equipment, prioritization of screening over other nursing tasks, and concerns the screening will not benefit patient care.4-6
We wished to understand if time and documentation are barriers to using geriatric screening tools in our ED. Our ED uses three screening tests for older adults, the Delirium Triage Screen (Delirium screen), 4 Stage Balance Test (4SBT)7, and Identifying Seniors at Risk (ISAR). These are simple, validated tools that can assist the provider with patient evaluation, optimization of care, and prevention of poor outcomes for the patient.8-12 The Delirium screen consists of a Richmond Agitation Sedation Scale (RASS) score and asking the patient to spell the word “LUNCH” backwards.8 The 4SBT is designed to assess static balance and involves having the patient stand up from the bed and complete four standing positions without an assistive device. ED patients who fail this screen are at increased risk of falling and may require additional resources aimed at improving strength and balance.9 Finally, the ISAR includes six questions which assess the care needs at home, hospitalizations, sensory or cognitive impairments, and medications.10 This screening tool can assist providers in recognizing the baseline functioning of an older adult presenting to the ED, identifying the need for specialty services, and considering referral for a full geriatric assessment.10,11 While these screening tests are designed to be quick and easy to administer, we found that at our institution, only 5% of eligible older adults who presented to the ED between January 2018 and August 2018 were screened. As part of an effort to address this implementation gap, we wanted to identify barriers to performing the screens.
To our knowledge, there have been no studies to assess the length of time needed to conduct the battery of geriatric screening tools recommended by the Geriatric ED Guidelines and analyze their impact on real workflow in the ED. While they may be quick to administer for a researcher, these screenings do not occur in a vacuum; rather, they are embedded in the context of the busy ED, to be performed by nurses who are managing multiple patients and tasks. Thus, we sought to better understand how much time the geriatric screens take a nurse to complete in the context of the ED, and what the barriers were to perform these screens in a real clinical environment.
Based on prior studies of implementing screening tools in the ED, we chose to evaluate the time needed to perform the screens, work interruptions, and the downstream ED workflow i.e., notification of providers regarding screening results. We designed a time workflow study to measure the time to conduct all three screening tools, assess for interruptions while performing the screens, and evaluate if providers were aware of where the results of the screens could be accessed and were using the information consistently.
Methods
Design and Study Setting
This was an IRB exempt study done for quality improvement purposes. Three trained observers (resident physicians in the ED and a medical student who are trained in geriatric screening assessments) shadowed nursing staff (n=27) during geriatric screening assessments for 30 encounters, including day and evening shifts. Observers were trained by LTS and the first five observations were done by dual observers to standardize observations. A standardized study sheet was designed to record timing of and barriers to screening. Screenings were completed on patients ≥65 years old in the ED and ED Observation Unit at an academic, tertiary care referral ED with 80,000 visits a year. The ED gained Level 1 Accreditation in August 2018 and the study was done in fall of 2018 as a quality assessment of the program.
Nurse Education and Training
As part of their role in this ED, nurses receive two hours of training in caring for older adults which includes how to perform and document the screens. Permission to be observed was asked of both the nurses and the patients; nurses were not blinded to being assessed. The nurses were asked to perform the screening assessments within view of the observer. As this was a QI endeavor, education was performed afterwards if there were any difficulties noted or questions arising during the screening process.
Observational Measures
A standardized observational protocol was developed to assess timing of each geriatric screening tool and interruptions. This was trialed with two nurses and feedback was used to adjust the protocol. Minutes in the ED prior to evaluation was calculated from ED bed placement. The start and stop times of each screening, and of the entire encounter, were recorded via stopwatch. Screens used were the Delirium Triage Screen (Delirium screen), Four Stage Balance Test (4SBT), and Identifying Seniors at Risk (ISAR).
1. Delirium Triage Screen
This screen focuses on patient attention and arousal. The screen was started when the nurse asked the patient to spell the word “lunch” backwards and ended when the patient had finished answering. During this time the nurse observed the patient to assign a RASS (Richmond Agitation-Sedation Score), from +4 ‘combative’ to -5 ‘unarousable’.
2. Four Stage Balance Test (4SBT)
This screening tool tests static balance. Patients were assessed for their ability to hold each of the following positions for 10 seconds: standing with feet side-by-side, placing one foot in the instep of the other, tandem stance, and standing on one foot (Figure 1). The 4SBT time started when the nurse began explaining the test positions or moved to the bedside to perform the assessment and ended when the patient had completed all positions. Time required to get the patient up and prepared for the balance testing, including any monitors or tethers that required removal, was also recorded.
3. Identifying Seniors At Risk (ISAR)
The ED form of the ISAR was used (Elder Alert Version). The questions include if the patient needed extra help at home prior to recent illness or injury, if they needed more help than usual due to recent illness or injury, recent hospitalizations, if they have eyesight problems, if they have memory problems, and if they are taking >5 medications per day. Patients were instructed to give yes or no answers. The ISAR time started when the nurse asked that first ISAR question and ended when the patient answered the last question.
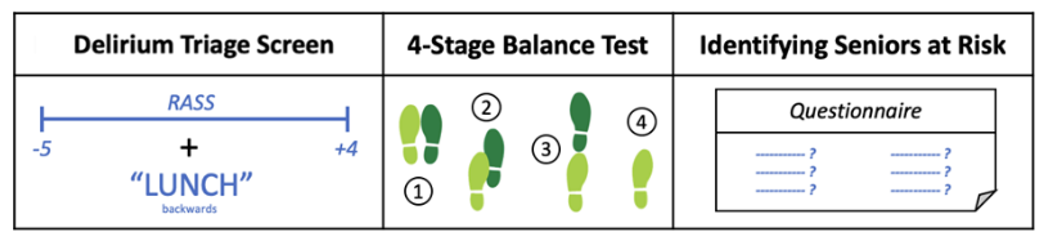 Figure 1: Screening tests administered for this workflow study: Delirium Triage Screen, 4-Stage Balance Test, Identifying Seniors at Risk.
Figure 1: Screening tests administered for this workflow study: Delirium Triage Screen, 4-Stage Balance Test, Identifying Seniors at Risk.
Documentation
Additional documentation time in the ED related to the screens was calculated from the time the nurse began documenting post-screening to when charting was complete. In addition, observers documented if the nurse informed the provider of any abnormal results related to the screens. The policy in place at the time was for the nurse to inform the provider of any abnormal screens and then the provider would order appropriate consultation (physical therapy, occupational therapy case manager, social worker, or geriatrics consultation). Providers (physicians, nurse practitioners, or physician assistants) caring for the patient were asked if they knew where in the electronic medical record (EMR) they could find results of the geriatric screening and subsequently educated on the location if unaware. Additionally, there is geriatric equipment available to assist with ambulation and delirium.13
Interruptions and Barriers
The observational protocol included space to document interruptions and disruptions such as phone calls and interruptions from patients, visitors, and staff. Any barriers to performing the assessments were also noted.
Analysis
Microsoft Excel was used to calculate mean and standard deviation of time in the ED, individual screening assessments, and proportion of screenings completed.
Results
Data was collected for a total of 30 geriatric screening observations with 27 ED nurses. On average, patients were in the ED for 8 hours and 52 minutes when the screening took place. The time to complete all screening assessments was 177±71 (mean±SD) seconds [range 69-297]. The total time to complete all three screening assessments was less than five minutes in all observations. The Delirium screen took 14±15 seconds [range 5-76] to complete. The time to stand the patient for the 4SBT was 20±27 seconds [range 1-123] while the time to complete the 4SBT was 58±28 seconds [range 6-142]. The ISAR was the most time-consuming portion of the assessment and took 81±40 seconds [range 36-216] to complete. Figure 2 depicts the average times and percent each screening took for the whole screening encounter. Interruptions occurred in three observations and all interruptions were initiated by patients asking questions about their medical care. The majority of nurses (24/30) documented concurrently while completing the assessments. In 4 observations, the nurse informed another team member of abnormal results of the screening. In 22 of the 30 observations, ED physicians/advanced practice practitioners were unaware of how to locate screening results in the EMR.
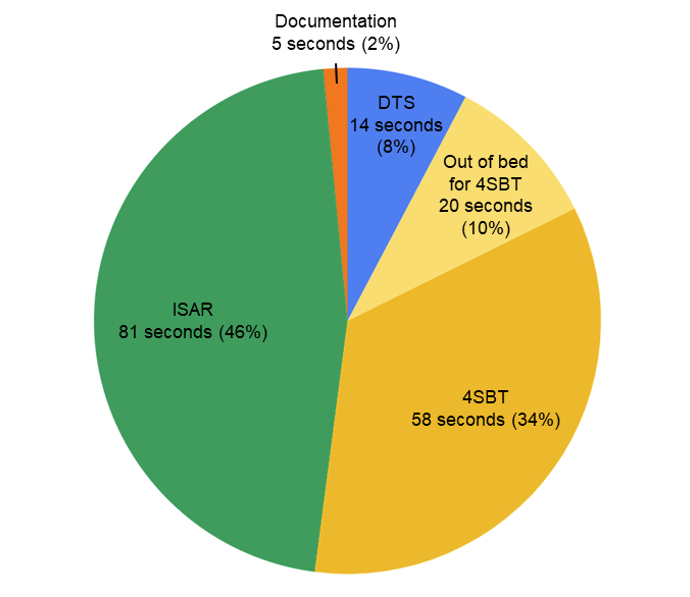 Figure 2: Average times to complete screenings and documentation. The Identifying Seniors at Risk (ISAR) screen took the longest, followed by the 4-Stage Balance Test (4SBT) and Delirium Triage Screen (DTS). Documentation was a minimal burden as it was most often performed concurrently with screening.
Figure 2: Average times to complete screenings and documentation. The Identifying Seniors at Risk (ISAR) screen took the longest, followed by the 4-Stage Balance Test (4SBT) and Delirium Triage Screen (DTS). Documentation was a minimal burden as it was most often performed concurrently with screening.
Discussion
We sought to gain an understanding of whether the time to complete geriatric assessments in a busy ED is a significant barrier to screening, and how these assessments may be incorporated into ED workflow. Performing three geriatric screening tools took ED nurses an average of three minutes of real clinical time, including interruptions and documentation. Interruptions were infrequent and documentation was usually completed concurrently and when performed separately added only a few seconds to the total assessment time. These geriatric screening tools provide a wealth of information about the needs of seniors seeking care in the ED and may identify the need for additional resources such as home health services, inpatient admission, or occupational and physical therapy. Our data suggest that performing these screenings is feasible in a busy ED.
This study did identify many barriers to screening. Anecdotally, the nurses perceived the screening as taking much longer than it actually did. They also felt that a large barrier was getting the patient up out of bed for the screening, but the actual time this took was 20 seconds on average. Future work should seek to better understand nurses’ perceptions of barriers to completing the screenings. For example, this perception may be due to their cognitive workload regarding competing demands with other patients. Additionally, we discovered on our trial tests of the observation protocol that it was important to remind the patient to only answer yes or no to the ISAR questions, or they frequently provided more detail than was needed for the screening process. While this was perceived as a barrier to the nurses, this could in fact provide more detail about the home health and safety needs of patients. One alternative would be to involve case managers in the ISAR screening who would be able to listen, elicit more information, and act on positive screens. Another direction for future research could involve utilizing patient responses to the ISAR with formulating a plan of care with colleagues from geriatrics, occupational therapy, physical therapy, and speech therapy.
The geriatric screening tests chosen for this ED were in part chosen due to their brevity. For example, we chose to use the 4SBT as a screening tool because it does not involve removing IVs, finding IV poles, or taking the patient off the cardiac monitor. If a balance/gait test that requires significant ambulation is chosen, such as the Timed Up and Go, the time to get the patient prepared and out of bed is likely to be more significant. Prior to this study, our team had trialed the Timed Up and Go and found that half of patients refused to get out of bed and ambulate for the test, due to monitors, illness, or other reasons. Consideration of the burden on staff and patients is needed prior to initiating a screening protocol in the ED.
We also identified a barrier to application of the geriatric assessment information. Most providers were unaware of where to find geriatric screening tool results in the EMR once they had been completed, and verbal communication about the results was rare. Since this study, our EMR has rolled out a chat function to allow the easy communication of non-critical information which has improved communication. We have also initiated an EMR dotphrase to pull the screen information into the provider note for easy analysis (Figure 3). This could overcome the barrier of difficulty finding the screening results in the EMR identified in this study. The patients were also getting screened near the end of their ED or ED Observation Unit stays, rather than the beginning, which suggests that this screening maybe seen as a box to check prior to disposition and not as critical to care planning. This culture will have to change with physicians as well to integrate the screening and actions on positive screens more fully into ED care.
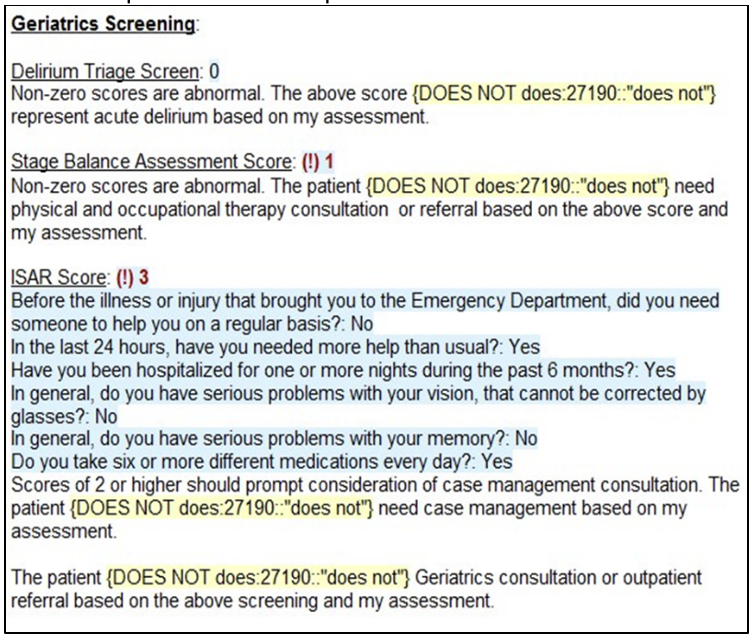 Figure 3: An Electronic Health Record dotphrase was created for providers to easily pull geriatric screening information into the provider notes. This was designed to solve the barrier of provider difficulty finding the screening information and to encourage consideration of consultation for abnormal results, with simple does or does not require consultation options.
Figure 3: An Electronic Health Record dotphrase was created for providers to easily pull geriatric screening information into the provider notes. This was designed to solve the barrier of provider difficulty finding the screening information and to encourage consideration of consultation for abnormal results, with simple does or does not require consultation options.
Limitations
Limitations of this study included direct observation of screenings by observers which may have caused the nurses completing the screenings to do so more quickly. Additionally, observation could have changed the patients’ behaviors and answers. Also, while the assessments were performed on different shifts over different days, selection bias may be present.
Conclusions
Performing three geriatric screening tools in a busy emergency department took an average of three minutes to perform, suggesting that these geriatric screening tools can be used without creating a significant bottleneck in ED workflow. Future steps for improvement include expansion to evaluate geriatric screening in differing ED sites, and evaluation of EMR tools to better encourage communication of screening results/actions.
Box 2: Study Recap
The challenge that led to this study
Screening tools for the geriatric emergency department populations are designed to be quick and easy to administer. In our institution, only 5% of geriatric patients were being screened. We sought to learn if time and documentation were barriers to completing the three geriatric ED screening tools.
The Key Findings or Points
Performing three geriatric screening tools took approximately three minutes to perform, and nurses overestimated the time burden involved in testing balance.
Implications for Clinical Practice
Geriatric screening tools can be performed quickly with minimal impact to nursing workflow in the ED. Further research is ongoing to evaluate the impact of geriatric screening on patient-centered outcomes.
Key Words
Screening, workflow, assessments, geriatrics, emergency
Acknowledgments
Co-Editors in Chief: Michael L. Malone, MD and Teresita M. Hogan, MD, FACEP
Conflict of Interest: Michael L. Malone owns stock in Abbott Labs and AbbVie.
The authors would like to thank all our ED nurses who provide great patient care and tolerated us following them around as well as Ariel Fuentes who assisted with data gathering.
Conflict of Interest
The authors have no conflict of interests to report. The authors have no external funding for this study.
Affiliations
Natalie M. Elder, MD, PharmD
- Department of Emergency Medicine, The Ohio State University, Columbus OH
Kimberly S. Bambach, MD
- Department of Emergency Medicine, The Ohio State University, Columbus OH
Megan E. Gregory, PhD
- Department of Biomedical Informatics, The Ohio State University, Columbus OH
- Center for the Advancement of Team Science, Analytics, and Systems Thinking in Health Services and Implementation Science Research, The Ohio State University College of Medicine, Columbus OH
Peg Gulker, MSN, RN
- College of Nursing, The Ohio State University, Columbus OH
Lauren T. Southerland, MD
- Department of Emergency Medicine, The Ohio State University, Columbus OH
References
- Apkan A, Roberts C, Bandeen-Roche K, et al. Standard set of health outcome measures for older persons. BMC Geriatr 2018;18:36. Doi: 10.1186/s12877-017-0701-3
- Rosenberg MS, Carpenter CR, Bromley M, et al. Geriatric emergency department guidelines. Ann Emerg Med 2014;63:e7-25. Doi: 10.1016/j.annemergmed.2014.02.008.
- Beach SR, Carpenter CR, Rosen T, et al. Screening and detection of elder abuse: Research opportunities and lessons learned from emergency geriatric care, intimate partner violence, and child abuse. J Elder Abuse Negl 2016;28:185-216. Doi: 10.1080/08946566.2016.1229241
- Carpenter CR, Griffey RT, Stark S, et al. Physician and nurse acceptance of technicians to screen for geriatric syndromes in the emergency department. West J Emerg Med 2011;12:489-495. Doi: 10.5811/westjem.2011.1.1962.
- Kirk JW, Silversten DM, Petersen J, et al. Barriers and facilitators for implementing a new screening tool in an emergency department: A qualitative study applying the Theoretical Domains Framework. J Clin Nurs 2016;25:2786-2797. Doi: 10.1111/jocn.13275.
- Tavender EJ, Bosch M, Fiander M, et al. Implementation research in emergency medicine: a systematic scoping review. Emerg Med J 2016;33:652-659. Doi: 10.1136/emermed-2015-205053.
- Southerland LT, Slattery L, Rosenthal JA, et al. Are triage questions sufficient to assign fall risk precautions in the ED? Am J Emerg Med 2017;35:329-332. Doi: 10.1016/j.ajem.2016.10.035.
- Han JH, Wilson A, Vasilevskis EE, et al. Diagnosing delirium in older emergency department patients: validity and reliability of the delirium triage screen and the brief confusion assessment method. Ann Emerg Med 2013:62,457-465. Doi: 10.1016/j.annemergmed.2013.05.003.
- Rossiter-Fornoff JE, Wolf SL, Wolfson LI, et al. A cross-sectional validation study of the FICSIT common data bases static balance measures. J Gerontol A Biol Sci Med Sci 1995;50:M291-297. Doi: 10.1093/gerona/50a.6.m291.
- McCusker J, Bellavance F, Cardin S, et al. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatric Soc 1999;47:1229-1237. Doi: 10.1111/j.1532-5415.1999.tb05204.x.
- Perry A, Macias Tejada J, Melady, D. An approach to the older patient in the emergency department. Clin Geriatr Med 2018;34:299-311. Doi: 10.1016/j.cger.2018.03.001.
- Melady D, Perry A. Ten best practices for the older patient in the emergency department. Clin Geriatr Med 2018;34:313-326. Doi: 10.1016/j.cger.2018.04.001.
- Southerland LT, Savage EL, Duff KM, et al. Hospital Costs and Reimbursement Model for a Geriatric Emergency Department. Acad Emerg Med 2020;27(10):1051-1058. Doi: 10.1111/acem.13998.
- Center for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Ensuring the COVID-19 Vaccines Work. Available at https://www.cdc.gov/coronavirus/2019-ncov/vaccines/effectiveness.html. Accessed December 14, 2020.
- Center for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Frequently asked questions about COVID-19 vaccination. Available at https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html. Accessed December 10, 2020.
- Center for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Ensuring the safety of COVID-19 vaccines in the United States. Available at https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety.html. Accessed December 10, 2020.