Can an Emergency Department Adequately Address an Older Adult who has Complex Needs?
Volume 2 | Issue 11 | Review Article
Download PDFIntroduction
The Emergency Department (ED) is a critical component of the geriatric continuum of care. Older adults comprise up to 25% of ED attendance and 38% of patients transported by emergency medical services (EMS.)2-4 Despite this, the traditional rapid linear ED treatment framework remains ill-equipped to meet the complex care needs of many vulnerable older adults.5-8 Upon discharge, the ED-to-home transition is a high-risk time for older adults. About one third of older adults will suffer an adverse result including ED revisit, eventual hospital referral, admission to a long-term care institution, or death within 3 months of the ED visit.9 Moreover, extended or frequent ED visits and repeated hospitalizations are costly. It has been reported that the cost of two potentially preventable geriatric syndromes, hospital delirium and repeated falls, is projected to be $83 billion a year in the United States.10,11
A Comprehensive Geriatric Assessment (CGA) is a framework to assess the medical, psychosocial, and functional challenges of older patients who have complex needs.12 The Acute Care for Elders model uses principles of CGA. Although CGA can be time intensive, a rapid assessment across multiple domains can be accomplished in the ED. The Domain Management Model (DMM) is an evaluation tool for providers to rapidly understand relevant factors driving the ED presentation within the domains. It is, essentially, a way to structure the “History of Present Illness” and “Social History” to capture complexity, expedite team communication, and facilitate transition planning.
In 2018, the American College of Emergency Physicians (ACEP) began accrediting facilities as “Geriatric Emergency Departments” (GEDs) in compliance with the multi-organizational recommendations released in 2014.13 However, despite broad circulation of the 2014 Consensus Geriatric ED recommendations, GED care remains heterogeneous, and the guidelines are not adopted in most EDs.14
We present this case scenario as a potentially avoidable admission. We explain how the Geriatric ED model using the ACE principles and the DMM approach may be employed to capture the important medical, cognitive, functional, and support environment details in the ED which allows for construction of a durable disposition plan.
Box 1: Case Description
An 80-year-old woman, with a medical history of dementia with behavioral changes, Parkinson’s disease, osteoporosis, chronic low back pain, and left leg sciatica presented to the ED by EMS for worsening acute on chronic pain and feeling of weakness in her legs. She “pulled” herself to one of the neighbors who called 911. During her ED evaluation, the patient was alert, calm, cooperative, and in moderate pain. Her vitals were stable. She was able to ambulate using a cane, with a shuffling gait, freezing, and stooped posture. Her general physical exam was otherwise normal. Her neurologic exam was not consistent with an acute neurological process. A Confusion Assessment Method (CAM) screening was negative for delirium. Her basic labs were normal. Imaging ruled out emergency pathology of the spinal cord. A prior MRI spine from one year prior detailed lumbar spondylosis and chronic T12 compression fracture. A quick chart review revealed recurrent ED visits. She had a total of five visits in two years resulting in three hospital admissions. Two hospitalizations were for acute-on-chronic leg pain and worsening gait. One hospitalization was for a non-syncopal fall resulting in a hand fracture. At every visit she was prescribed a different pain management regimen. Each regimen had been discontinued because it was not effective or not tolerated due to side effects. She was maintained on pregabalin without obvious improvement in her feet pain. On a recent clinic visit, her primary care provider (PCP) added duloxetine for depression. There was no Geriatric ED program at the site. As it was deemed too risky to return her to her home environment in her current condition, and her multiple chronic conditions couldn’t be addressed in the emergency department, the ED team decided to admit her to the ACE unit for further interdisciplinary evaluation and management.
Discussion
We describe below three approaches to the acute care of older adults. These illustrate how geriatric principles may be applied to ED patients with multimorbidity and complex needs to reduce potentially avoidable hospitalizations. The strategies include: the geriatric ED model replicating ACE principles, the Domain Management Model, and the use of screening tools for common geriatrics syndromes. There is overlap of geriatric principles with each model.
Geriatric ED Model
The inpatient ACE unit model involves a multidisciplinary team utilizing a structured approach to comprehensive assessment, team and family communication, and proactive disposition planning.15,16 Members may include a geriatrician, a transitional nurse (TCN) or a geriatric nurse practitioner (NP), a social worker (SW), a pharmacist, a physical therapist (PT), and palliative care consultants. These members collaboratively develop a goal-concordant, patient-centered care, and disposition plan. The geriatric ED model involves systematized, holistic evaluation and targeted interdisciplinary discussions for high-risk patients, effectively mirroring the ACE process in the time-pressured, limited-resource ED environment. As a full multidisciplinary team is seldom available in the ED, providers and nurses may approximate an ACE assessment utilizing the Domain Management Model and select screening instruments.
Domain Management Model
This efficient paradigm is the model that guides the ED team to capture, arrange, and communicate complexities across disciplines, specialties, and care sites. It evaluates across four domains: medical/surgical issues, mental status/cognition, physical function, and physical/social/financial living environment.17,18
- The first domain consists mainly of acute medical management: identifying comorbid diseases, medication management, and facilitating medical transitions of care.
- The second domain is important to recognize cognitive impairment (dementia, delirium) and associated psychological or behavioral problems.
- The third domain addresses baseline functional status, screening for functional decline, and fall risk.
- The fourth domain evaluates the living arrangements of the older adult (situation and home safety), social support systems (family members, care givers, elder abuse risk, community resources), and financial management (e.g., exploitation risk.)
ED-Based Screening Tools
ED-based screening for high-risk features complements the Domain Management model and may reduce the risk of potentially avoidable adverse outcomes during and shortly after the ED visit. Serious geriatric syndromes such as delirium, dementia, and functional impairment are often not identified in the standard ED evaluation, with subsequent effects on length of stay, mortality, and readmission. Processes and systems can be implemented into ED workflow to make screening feasible, reducing risk through timely diagnosis and management, as well as linkage to appropriate services beyond the ED.
Box 2: Comprehensive Geriatric Assessment using Domain Management Model in Geriatric ED and ACE Unit
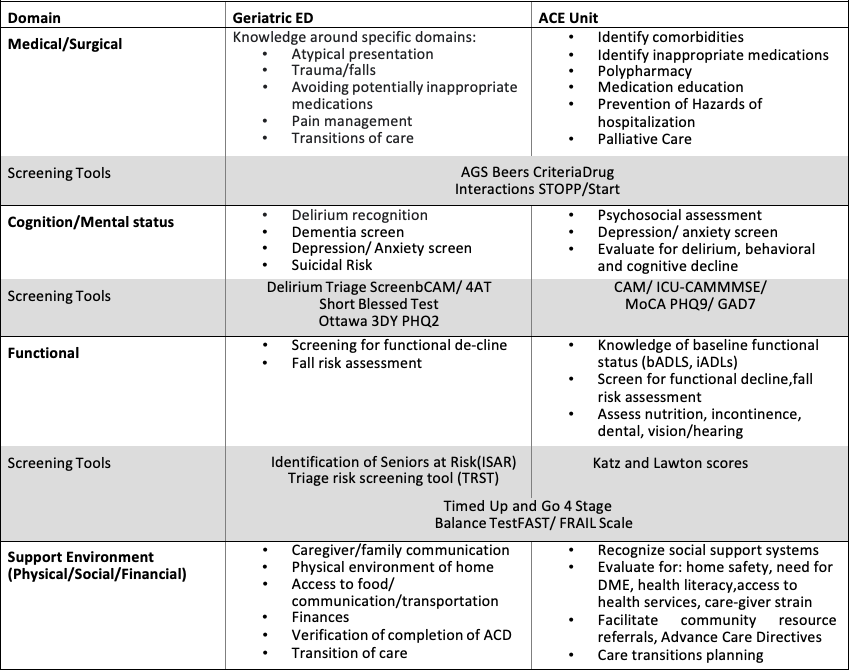
Box 2 uses the Domain Management Model to describe key strategies of the Geriatric ED and ACE unit, respectively. Some screening tools are applicable in each setting to assess the older patients’ unique needs and their specific goals.19 Screening in the Geriatric ED is performed by the nursing staff and further assessment follows.20
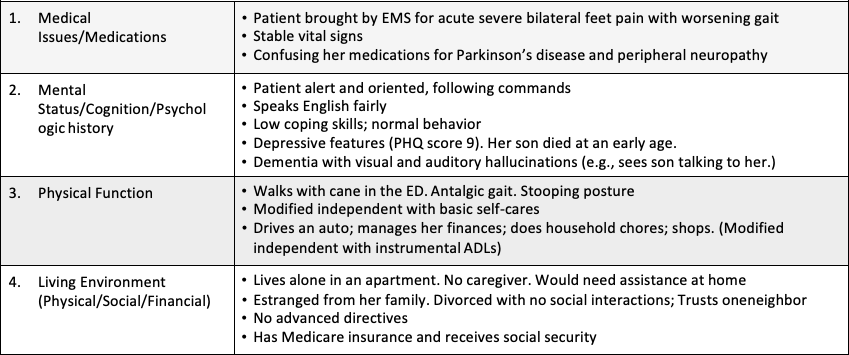
Box 3 provides an example on how we can apply the Domain Management Model in the ED in the context of this patient’s case.
Box 3: Application of the Domain Management Model in ED to This Case
Box 4: Case Follow-Up
The ACE unit interdisciplinary team determined that the patient had been confusing her medications. She mistakenly took extra doses of her Parkinson medications, which interfered with her peripheral neuropathy symptoms. A geropsychiatric examination confirmed cognitive dysfunction (MoCA score of 18 of 30) and depression (PHQ score of 9). The patient had long standing sleeping problems and depressive psychosis with visual and auditory hallucinations of her long- deceased son who tragically committed suicide in his early adulthood. She also had delusions that her physicians and people surrounding her had intentions to hurt her. These delusions interfered with her medication adherence and her trust in her primary care physician. She was independent in her basic self-cares (ADL’s Katz score:6/6, IADL Lawton score:8/8). She had no advance directives. The ACE unit team also determined that while the patient could speak and understand English, she could neither read nor write English. Her English proficiency hindered her understanding of “after visit summaries,” discharge instructions, and safe medication use.
On further investigation of the patient’s social background, she endorsed strong cultural and religious beliefs. She was alone with no social connections. Her assessment occurred over the first 48 hours of her care. Following her discharge from the hospital, a home visit was conducted by a transitional care nurse. This nurse scheduled appointments with her primary care provider, a geriatric psychiatrist, and home care services (including a home health aide.) The home health social worker engaged the adult protective services for guardianship assignment and communicated some resources to the patient for surrounding Korean communities. The patient’s understanding of her medications was confirmed and monitored.
Summary
Evaluating the needs of older adults who have complex needs in the ED is a unique challenge. It takes considerable time to gather information from the patient and their caregivers, and to review a long medical history and medication list. The provider must determine the new and the baseline findings and integrate that information with data obtained during the ED evaluation. Older patients who have complex needs are often simply admitted to the hospital or are sent to an observation unit to sort out multiple medical, cognitive, and functional issues. The interdisciplinary approach of the geriatric ED uses principles of the acute care for elders (ACE) model and integrates geriatric screening tools that were previously used in the context of hospital care. Other frameworks were also designed for a comprehensive geriatric evaluation, including the Geriatric 5Ms model of care addressing 5 domains: Mind, Mobility, Medications, Multi-Complexity, and What Matters Most. Similarly, the Domain Management Model uses a holistic systematic approach to assess multiple aspects of an older patient’s needs. This approach can help the team to develop a care plan which may allow an individual to avoid hospitalization.
Key Words
Geriatric emergency care, domain management model, transitional care, ACE model
AFFILIATIONS
Rami Tarabay, MD
Department of Geriatrics, MetroHealth Case Western Reserve University Program, Cleveland, Ohio
Adam Perry, MD
Geriatric Emergency Department Collaborative
Riwa Al Aridi, PharmD
Faculty of Pharmacy, Lebanese International University, Beirut, Lebanon
Michael Malone, MD
Department of Geriatrics, Advocate Aurora Health, Director Senior of Services, Wisconsin
AUTHOR CONTRIBUTIONS
RT, MM: conceptualization of the case scenario. RT, MM, AP, RA: Drafting the original manuscript and literature review. MM, AP: Supervision, review and editing. All authors read and approved the final manuscript.
NAME AND CONTACT INFORMATION OF THE CORRESPONDING AUTHOR
Michael L. Malone, MD: (414) 588-2991, Email: michael.malone.md@aah.org
CONFLICTS OF INTEREST
Michael L. Malone owns stock in Abbott Labs and Abbvie. The authors have declared no conflicts of interest for this article.
ACKNOWLEDGEMENTS
This case was presented in the national most difficult case presentation series and was described in an abstract for the American Geriatric Society 2021 annual meeting.
References
- U.S. Census Bureau. Selected Social Characteristics in the United States (Online). https://data.cen- sus.gov/cedsci/table?q=Selected Social Characteristics in the United States &tid=ACSDP1Y2019.DP02&hidePreview=false. Accessed February 7, 2021.
- Legramante JM, Morciano L, Lucaroni F, et al. Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established. Bugiardini R, ed. PLoS One. 2016;11(12):e0165939. doi:10.1371/journal.pone.0165939
- Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: A re- view. Ann Emerg Med. 2010;56(3):261-269. doi:10.1016/j.annemergmed.2010.04.015
- Evans CS, Platts-Mills TF, Fernandez AR, et al. Repeated Emergency Medical Services Use by Older Adults: Analysis of a Comprehensive Statewide Database. Ann Emerg Med. 2017;70(4):506- 515.e3. doi:10.1016/j.annemergmed.2017.03.058
- Lennox A, Braaf S, Smit DV, Cameron P, Lowthian JA. Caring for older patients in the emergency department: Health professionals’ perspectives from Australia – The Safe Elderly Emergency Discharge project. EMA – Emerg Med Australas. 2019;31(1):83-89. doi:10.1111/1742-6723.13108
- Disseminating and Sustaining Emergency Department Innovations for Older Adults: Good Ideas Deserve Better Policies. 2017. doi:10.1111/acem.13339
- Hwang U, Morrison RS, Lillian Z, Hertzberg B. The Geriatric Emergency Department. J Am Geri- atr Soc. 2007;55:1873-1876. doi:10.1111/j.1532-5415.2007.01400.x
- Hwang U, Shah MN, Han JH, Carpenter CR, Siu AL, Adams JG. Transforming emergency care for older adults. Health Aff. 2013;32(12):2116-2121. doi:10.1377/hlthaff.2013.0670
- Hastings SN, Oddone EZ, Fillenbaum G, Sloane RJ, Schmader KE. Frequency and predictors of adverse health outcomes in older medicare beneficiaries discharged from the emergency depart- ment Med. Care 46 771–7Frequency and predictors of adverse. Med Care. 2008;46(8):771-777. doi:10.1097/MLR.0b013e3181791a2d
- Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs as- sociated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27-32. doi:10.1001/ archinternmed.2007.4
- Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Non- fatal Falls in Older Adults. J Am Geriatr Soc. 2018;66(4):693-698. doi:10.1111/jgs.15304
- Ellis G, Marshall T, Ritchie C. Comprehensive geriatric assessment in the emergency department. Clin Interv Aging. 2014;9:2033-2044. doi:10.2147/CIA.S29662
- ACEP Accredits Geriatric Emergency Care for Emergency Departments – ACEP Now. https:// www.acepnow.com/article/acep-accredits-geriatric-emergency-care-emergency-departments/. Ac- cessed February 7, 2021.
- Carpenter CR, Bromley M, Caterino JM, et al. Optimal older adult emergency care: Introducing multidisciplinary geriatric emergency department guidelines from the American College of Emer- gency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine. J Am Geriatr Soc. 2014;62(7):1360-1363. doi:10.1111/jgs.12883
- Flood KL, MacLennan PA, McGrew D, Green D, Dodd C, Brown CJ. Effects of an acute care for elders unit on costs and 30-day readmissions. JAMA Intern Med. 2013;173(11):981-987. doi:10.1001/jamainternmed.2013.524
- Barnes DE, Palmer RM, Kresevic DM, et al. Acute care for elders units produced shorter hospital stays at lower cost while maintaining patients’ functional status. Health Aff. 2012;31(6):1227-1236. doi:10.1377/hlthaff.2012.0142.
- Siebens H. The domain management model- A tool for teaching and management of older adults in emergency departments. Academic Emergency Medicine 2005;12(2): 162-168.
- Kushner DS, Peters KM, Johnson-Greene D. Evaluating use of the Siebens Domain Management Model during inpatient rehabilitation to increase functional independence and discharge rate to home in stroke patients. PM R. 2015 Apr;7(4):354-64. doi: 10.1016/j.pmrj.2014.10.010.
- Megalla M, Avula R, Manners C et al. Using the 4M Model to Screen Geriatric Patients in the Emergency Department, Journal of Geriatric Emergency Medicine. 2021; 2(9): Article 1. Available at: https://institutionalrepository.aah.org/jgem/vol2/iss9/1.
- Southerland LT, Stephens JA, Carpenter C, et al. Study protocol for IMAGE: Implementing multi- disciplinary assessments for geriatric patients in an emergency department observation unit, a hy- brid effectiveness/ implementation study using the Consolidated Framework for Implementation Research. Implementation Science Communications 2020; 1:28. https://doi.org/10.1186/s43058-020-00015-7