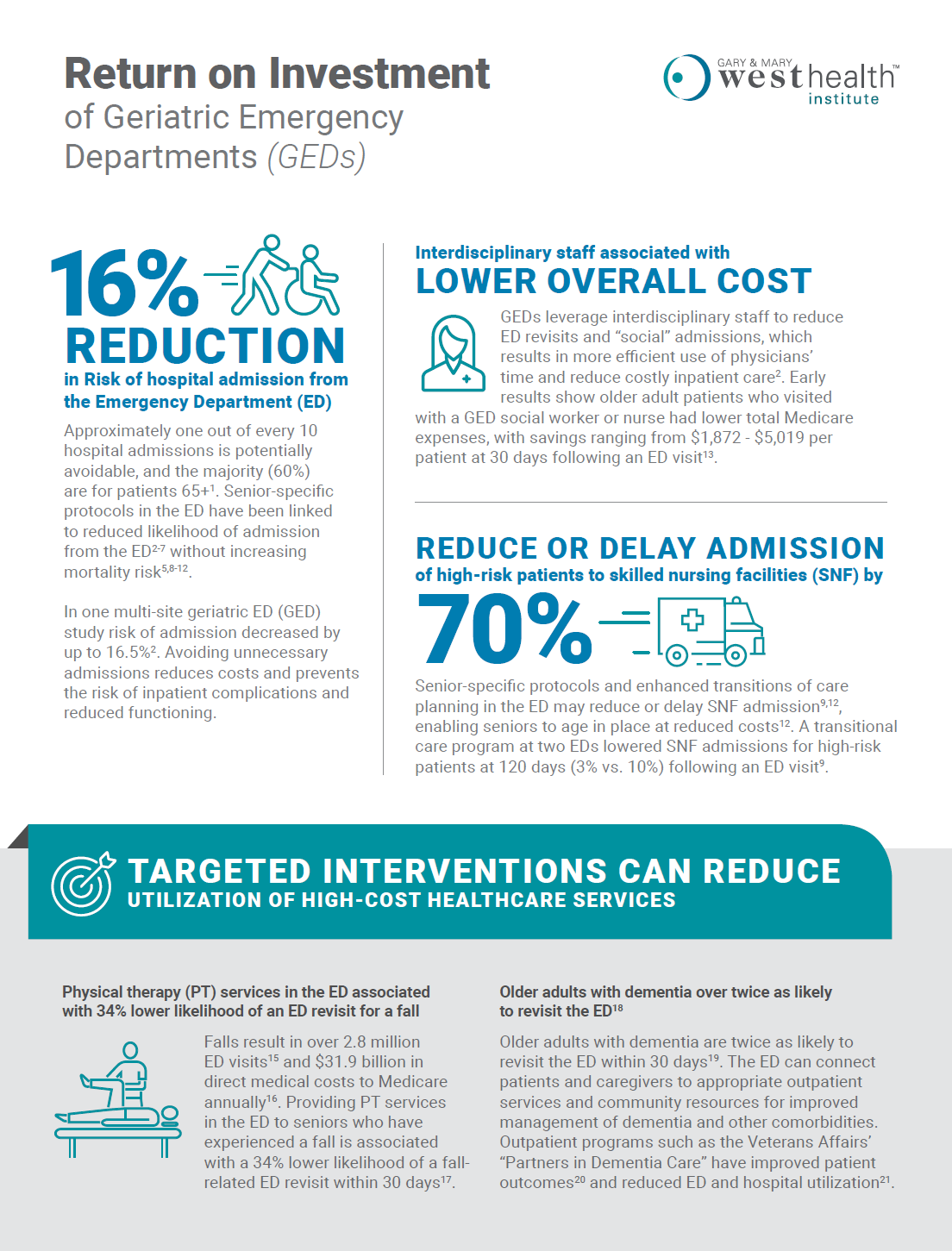
16% Reduction in risk of hospital admission from the Emergency Department (ED)
Approximately one out of every 10 hospital admissions is potentially avoidable, and the majority (60%) are for patients 65+1. Senior-specific protocols in the ED have been linked to reduced likelihood of admission from the ED2-7 without increasing mortality risk5,8-12.
In one multi-site geriatric ED (GED) study risk of admission decreased by up to 16.5%2. Avoiding unnecessary admissions reduces costs and prevents the risk of inpatient complications and reduced functioning.
Interdisciplinary staff associated with lower overall cost
GEDs leverage interdisciplinary staff to reduce ED revisits and “social” admissions, which results in more efficient use of physicians’ time and reduce costly inpatient care2. Early results show older adult patients who visited with a GED social worker or nurse had lower total Medicare expenses, with savings ranging from $1,872 – $5,019 per patient at 30 days following an ED visit13.
Reduce or delay admission of high-risk patients to skilled nursing facilities (SNF) by 70%
Senior-specific protocols and enhanced transitions of care planning in the ED may reduce or delay SNF admission9,12, enabling seniors to age in place at reduced costs12. A transitional care program at two EDs lowered SNF admissions for high-risk patients at 120 days (3% vs. 10%) following an ED visit9.
Targeted interventions can reduce utilization of high-cost healthcare services
Physical Therapy
Physical therapy (PT) services in the ED associated with 34% lower likelihood of an ED revisit for a fall.
Falls result in over 2.8 million ED visits15 and $31.9 billion in direct medical costs to Medicare annually16. Providing PT services in the ED to seniors who have experienced a fall is associated with a 34% lower likelihood of a fall-related ED revisit within 30 days17.
Older Adults with Dementia
Older adults with dementia over twice as likely to revisit the ED18
Older adults with dementia are twice as likely to revisit the ED within 30 days19. The ED can connect patients and caregivers to appropriate outpatient services and community resources for improved management of dementia and other comorbidities.
Outpatient programs such as the Veterans Affairs’ “Partners in Dementia Care” have improved patient outcomes20 and reduced ED and hospital utilization21.
Sources
1Stranges E, Stocks C. Potentially Preventable Hospitalizations for Acute and Chronic Conditions, 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2010.
2Hwang U, Dresden SM, Rosenberg MS, et al. Geriatric Emergency Department Innovations: Transitional Care Nurses and Hospital Use. Journal of the American Geriatrics Society. 2018;66(3):459-466.
3Aldeen AZ, Courtney DM, Lindquist LA, et al. Geriatric Emergency Department Innovations: Preliminary Data for the Geriatric Nurse Liaison Model. Journal of the American Geriatrics Society. 2014;62(9):1781-1785.
4Keyes DC, Singal B, Kropf CW, et al. Impact of a New Senior Emergency Department on Emergency Department Recidivism, Rate of Hospital Admission, and Hospital Length of Stay. Annals of Emergency Medicine. 2014;63(5):517-524.
5Wallis M, Marsden E, Taylor A, et al. The Geriatric Emergency Department Intervention model of care: a pragmatic trial. BMC Geriatrics. 2018;18(1):297.
6Conroy SP, Ansari K, Williams M, et al. A controlled evaluation of comprehensive geriatric assessment in the emergency department: the ‘Emergency Frailty Unit’. Age and Ageing. 2014;43(1):109-114.
7Wright PN, Tan G, Iliffe S, et al. The impact of a new emergency admission avoidance system for older people on length of stay and same-day discharges. Age and Ageing. 2014;43(1):116-121.
8Silvester KM, Mohammed MA, Harriman P, et al. Timely care for frail older people referred to hospital improves efficiency and reduces mortality without the need for extra resources. Age and Ageing. 2014;43(4):472-477.
9Mion LC, Palmer RM, Meldon SW, et al. Case finding and referral model for emergency department elders: A randomized clinical trial. Annals of Emergency Medicine. 2003;41(1):57-68.
10Caplan GA, Williams AJ, Daly B, et al. A Randomized, Controlled Trial of Comprehensive Geriatric Assessment and Multidisciplinary Intervention After Discharge of Elderly from the Emergency Department—The DEED II Study. Journal of the American Geriatrics Society. 2004;52(9):1417-1423.
11Miller DK, Lewis LM, Nork MJ, et al. Controlled Trial of a Geriatric Case-Finding and Liaison Service in an Emergency Department. Journal of the American Geriatrics Society. 1996;44(5):513-520.
12Ellis G, Whitehead MA, Robinson D, et al. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343.
13Carter MW, Datti B, Winters JM. ED visits by older adults for ambulatory care-sensitive and supply-sensitive conditions. The American Journal of Emergency Medicine. 2006;24(4):428-434.
14Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years — United States, 2014. Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report. 2016;65(37):993–998
15Burns E, Stevens J, Lee R. The direct costs of fatal and nonfatal falls among older adults – United States. J Safety Res. 2016;58:99-103.
16Lesser A, Israni J, Kent T, et al. Association Between Physical Therapy in the Emergency Department and Emergency Department Revisits for Older Adult Fallers: A Nationally Representative Analysis. Journal of the American Geriatrics Society. 2018;66(11):2205-2212.
17Wolinsky FD, Liu L, Miller TR, et al. Emergency Department Utilization Patterns Among Older Adults. The Journals of Gerontology: Series A. 2008;63(2):204-209.
18LaMantia MA, Stump TE, Messina FC, et al. Emergency Department Use Among Older Adults With Dementia. Alzheimer disease and associated disorders. 2016;30 (1):35-40.
19Bass DM, Judge KS, Snow AL, et al. A controlled trial of Partners in Dementia Care: veteran outcomes after six and twelve months. Alzheimer’s research & therapy. 2014;6 (1):9-9.
20Bass DM, Judge KS, Maslow K, et al. Impact of the care coordination program “Partners in Dementia Care” on veterans’ hospital admissions and emergency department visits. Alzheimer’s & Dementia: Translational Research & Clinical Interventions. 2015;1(1):13-22.
21Hwang U, Dresden S, Garrido M, et al. Geriatric Emergency Department (ED) Innovations: ED-based Social Work associated with reduced Medicare expenditures. Paper presented at: American Geriatrics Society Annual Meeting 2018.